Abstract
Introduction
Naturally occurring regulatory (Treg) cells expressing the transcription factor FoxP3 are actively engaged in the maintenance of immunological self-tolerance and homeostasis. On the other hand, they are hindering effective anti-tumor immune responses in cancer patients, indicating possible augmentation of tumor immunity by depletion of FoxP3+ Treg cells. Here we show that this can be achieved by imatinib, a tyrosine kinase inhibitor of the oncogenic BCR-ABL fusion protein specifically expressed in chronic myelogenous leukemia (CML) cells.
Methods
Peripheral blood samples were obtained from healthy individuals and CML patients. PBMCs were directly subjected to ex vivo staining for the analyses of FoxP3+CD4+ T cells and activation status of CD8+ T cells. Cytokine production by CD8+ T cells was detected by intracellular cytokine staining after stimulation with PMA/Ionomycin using BD Cytofix/Cytoperm Fixation/Permeabilization Kit. To detect the effect of TKI on T cells, CFSE-labelled CD8+ T cells, CD45RA+CD25lo nTreg cells, CD45RA-CD25hi eTreg cells and CD25- T cells were stimulated for 5 days with Dynabeads Human T-Activator CD3/CD28 (Life technologies) in the presence/absence of imatinib, nilotinib or dasatinib, and then assessed for proliferation and induction of apoptosis. Flow cytometric analyses were performed with an LSR Fortessa (BD Bioscience) and analysed with FlowJo Version 9.6.2 software. For investigation of imatinib target(s), expression levels of mRNA, and total and phosphorylated protein by sorted CD8+ T cells, CD45RA+CD25lo nTreg cells, CD45RA-CD25hi eTreg cells and CD25- T cells were analysed by standard quantitative real-time PCR and western blotting.
Results
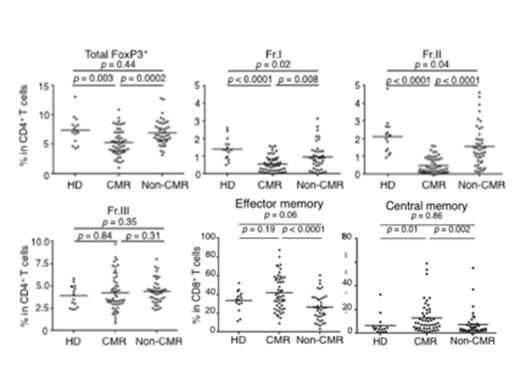
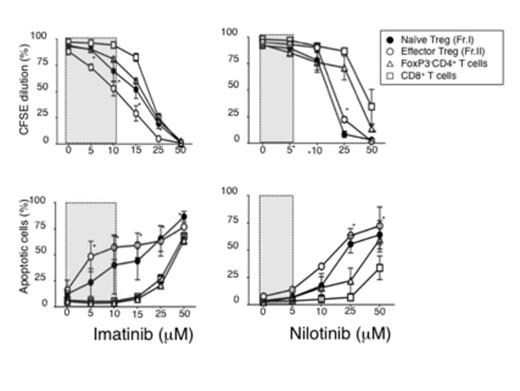
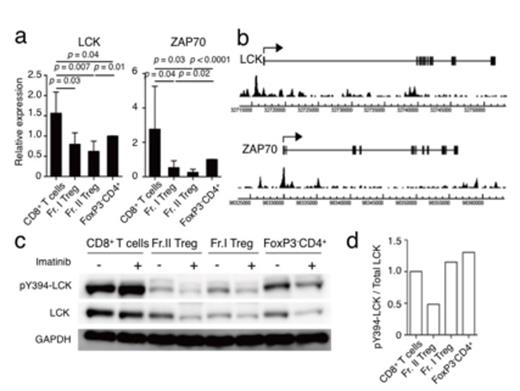
Long-term imatinib-treated CML patients in complete molecular remission with no detection of BCR-ABL mRNA in the blood cells showed selective depletion of terminally differentiated and highly suppressive FoxP3+ effector Treg cells whereas those not in molecular remission did not (Figure1). The former concurrently exhibited a general increase in the number of effector- or memory-type CD8+ T cells producing multiple cytokines. In vitro, imatinib induced apoptosis predominantly in effector Treg cells, augmenting CD8+ T-cell responses against various tumor antigens in healthy individuals and cancer patients (Figure 2). It inhibited tyrosine phosphorylation of LCK (lymphocyte-specific protein tyrosine kinase), a T cell-specific signaling molecule, as an off-target effect. In Treg cells, FoxP3-dependent gene repression maintained at low levels the expression of LCK and its down-stream signaling molecule zeta-chain-associated protein kinase 70 (ZAP-70) (Figure 3).
Conclusion
Imatinib is, therefore, able to attenuate T-cell receptor (TCR) signaling intensity more profoundly in Treg cells than in other T cells, rendering the former more susceptible to signal-deprived apoptotic cell death. Thus, small molecules that can selectively deplete Treg cells via exploiting FoxP3-dependent Treg-cell functions are instrumental in evoking and augmenting anti-tumor immunity against various cancers.
Takahashi:Celgene: Speakers Bureau; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Sysmex: Research Funding, Speakers Bureau; Masis: Consultancy; Otsuka: Membership on an entity's Board of Directors or advisory committees; BMS: Honoraria, Research Funding, Speakers Bureau; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Astellas: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal