Abstract
BACKGROUND AND AIMS
Allogeneic bone marrow transplantation (BMT) offers the greatest chance of cure for patients with high-risk acute myeloid leukemia (AML). Persistence of disease or high levels of pre BMT minimal residual disease (MRD) have been reported to predict relapse risk after BMT. WT1 expression levels and multicolor flow cytometry (MFC) are the most common tools to evaluate MRD. We recently reported that combining WT1 expression and MFC for MRD detection after induction therapy strongly impacts on relapse risk in AML. The aim of this study was to analyze the role of pre-BMT MRD assessment as predictor for the post-transplant relapse risk.
MATERIALS AND METHODS
We retrospectively analyzed the outcome of 253 consecutive AML patients receiving allo-BMT. Pre-BMT marrow samples were analysed for WT1 expression and MFC as MRD evaluation . Median age at transplant was 45 years. Disease phase was CR1 in 161, CR2 in 63, and CR3 in 29 patients. One hundred eighty-two received myeloablative conditioning, whereas 71 patients received reduced intensity conditioning. Median follow-up was 59 months (95% CI 46.2 - 71.8 months). Relapse-free survival (RFS) was calculated from the time of transplantation until last follow-up or documented leukemic relapse. Overall Survival (OS) was calculated from the time of transplantation until death by any cause or last follow-up.
A positive MFC MRD was defined by the presence of no less than 25 clustered leukemic cells/105 total events (threshold of 2.5x10-4 residual leukemic cells) at four-color flow-cytometry. Real-time PCR for WT1 was performed on DNA Engine 2 (Opticon®, MJ Research®). WT1 copy number/Abl copy number 500x104 was used as cut-off value for abnormal WT1 expression.
RESULTS
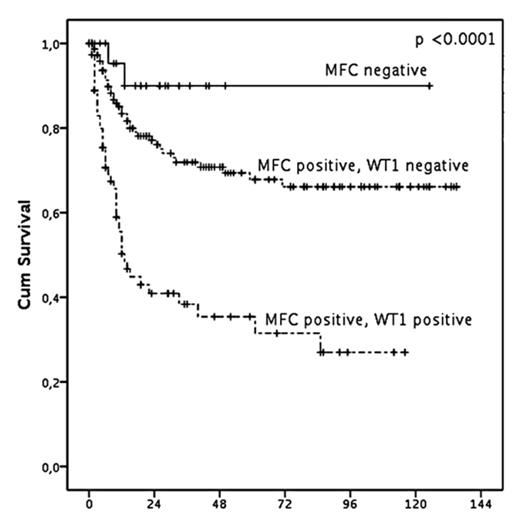
Relapse occurred in 81 patients (32%). Three-year estimate of RFS was 63.7% (median not reached). The probability of relapse was significantly affected by disease status (first or subsequent CR, p<0.01), occurrence of acute GVHD (grade 0-1 versus 2 or more, p <0.05), MRD status before transplantation, measured with any method (p <0.001 for WT1-based MRD, p<0.03 for MFC based MRD, p<0.0001 for combined MRD). Multivariate RFS analysis revealed that the combined MRD evaluation was the only independent predictor of RFS (p <0.001).
Specifically, MFC-MRD was the strongest predictor of longer relapse free survival (p <0.001) since only two relapses occurred in the 25 MFC-MRD negative patients and 3-years RFS was 89.9%. Among MFC-MRD positive patients, WT1 MRD status stratified the risk of relapse as the 3-years RFS was 71.9% and 31.3%, respectively, for patients with normal or increase WT1, p <0.01, fig.1). The predictive value of MRD was independent from induction schedules, donor type, disease status at BMT and risk group, occurrence of acute or chronic GVHD. Similarly, MRD evaluation was a strong predictor of long term survival, as 3- years OS was 77.2% for MFC negative and 36.9% for double WT1 and MFC MRD positive patients, respectively, (p <0.001). Multivariate OS analysis showed that BMT year, disease status at BMT and combined MRD evaluation significantly influenced OS duration (p <0.001, <0.002 and <0.003, respectively)
CONCLUSIONS
Pre transplant MRD evaluation by WT1 and MFC on bone marrow samples is a reliable predictor of relapse risk. Patients with both negative pre-BMT MRD markers have a significantly longer RFS, while patients with both positive MRD markers display an higher risk of relapse. Identifying patients who have an higher risk of relapse could open the way to apply pre-emptive therapeutic strategies to prevent AML relapse, from donor lymphocyte infusion to other innovative approaches.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal