Abstract
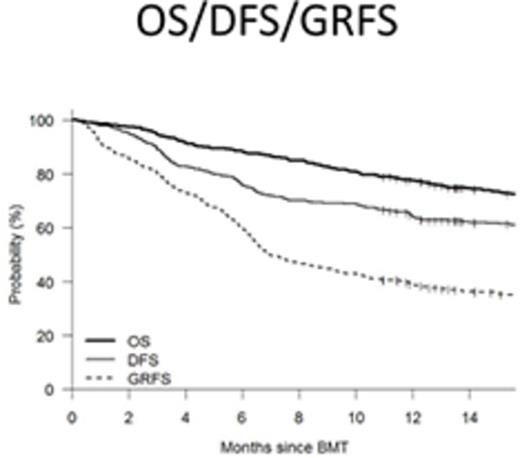
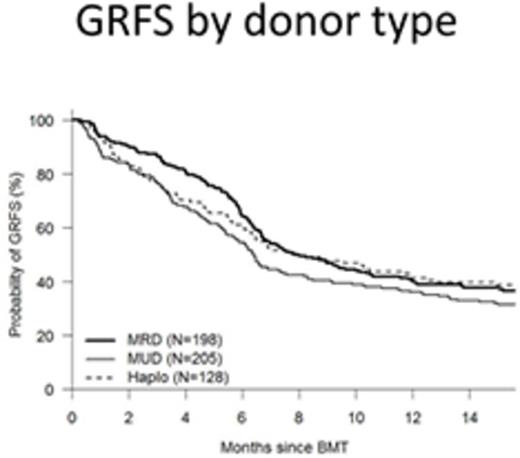
The ideal outcome of allogeneic hematopoietic cell transplantation (allo-HCT) is based on survival that is free of morbidity. The most common causes of treatment failure and morbidity after HCT are relapse, GVHD and non-relapse death. A composite endpoint that measures survival free of clinically significant negative events may be a useful way to determine the success of allo-HCT (1). We assessed GVHD and relapse-free survival (GRFS) where the events were acute GVHD grade 3-4, moderate to severe chronic GVHD, relapse or death in 531 consecutive adult patients who received an allo- HCT between 2006 and 2014 at our center. Median follow up of living patients was 46 months (12-123). Patients were treated using standardized supportive care algorithms at our center. Although this was a retrospective analysis, patient characteristics and outcomes including GVHD grading were obtained from our institutional database where they had been prospectively documented. The median age was 52 (18-77) years. 266 (50%) received myeloablative conditioning, and 428 (81%) received PBSC as stem cell source. Donor type was HLA matched related (MRD, n=198, 37%), matched unrelated (MUD, n=205, 39%) and haploidentical using T-replete grafts and post-transplant cyclophosphamide (HIDT, n=128, 24%). 36% of patients had a high/very high Dana farber disease risk index (DRI). The most common indications for transplant were AML (n=197, 37%), MDS/MPS (n=114, 21%), NHL (n=132, 25%) and ALL (n=68, 13%).1 year OS, disease free survival DFS and GRFS were 78%, 64% and 33% respectively. GRFS after MRD, MUD and HIDT was 39%, 27% and 35% respectively, with MRD recipients having a better GRFS than MUD (p=0.004). Regression analysis showed that GRFS at the one year was lower for, patients transplanted before 2011 than those transplanted between 2011 and 2014(27% vs 39%, p=0.0031), high CIBMTR disease risk than low CIBMTR risk (24% vs 39%, p=0.009) and high/very high DRI than low DRI (23% vs 48%, p<0.001). On multivariable analysis, year of transplant before 2011 (HR =1.2, p=0.03), age >= 50 years (HR 1.22, p=0.05), MUD donor (HR 1.3, p=0.004) and high/very high DRI risk (HR 2.05, p<0.001) were all associated with a worse GFRS at one year post HCT.
GFRS is an endpoint that is worth investigating in further trials as a marker of successful HCT. These data suggest that GRFS can be predicted by patient age and DRI but not by HCT-CMI. Importantly the GRFS appears to have improved in more recently transplanted patients and MUD donors produce inferior GRFS to MRD whereas haploidentical donors do not.
Predictors of GRFS at one year
| . | N=531 . | 1 year GRFS . | HR . | 95% CI . | P value . |
|---|---|---|---|---|---|
| Year of BMT 2005-2010 2011-2014 | 270 (51%) 261 (49%) | 30% 37% | 1.00 0.80 | 25%-35% 32%-43% | - 0.03 |
| Age Age <50 years Age >= 50 years | 228 (43%) 303(57%) | 37% 31% | 1.00 1.22 | 31%-43% 26%-36% | - 0.05 |
| Donor Type MRD MUD Haplo Haplo vs MUD | 198(37%) 205 (39%) 128 (24%) | 39% 27% 35% | 1.00 1.30 1.13 0.81 | 33%-45% 22%-33% 27%-42% | - 0.004 0.379 0.112 |
| DRI Low Intermediate High/very high | 78(15%) 258 (49%) 189 (36%) | 48% 36% 23% | 1.00 1.42 2.05 | 38%-58% 31%-42% 18%-29% | - 0.025 <0.001 |
| . | N=531 . | 1 year GRFS . | HR . | 95% CI . | P value . |
|---|---|---|---|---|---|
| Year of BMT 2005-2010 2011-2014 | 270 (51%) 261 (49%) | 30% 37% | 1.00 0.80 | 25%-35% 32%-43% | - 0.03 |
| Age Age <50 years Age >= 50 years | 228 (43%) 303(57%) | 37% 31% | 1.00 1.22 | 31%-43% 26%-36% | - 0.05 |
| Donor Type MRD MUD Haplo Haplo vs MUD | 198(37%) 205 (39%) 128 (24%) | 39% 27% 35% | 1.00 1.30 1.13 0.81 | 33%-45% 22%-33% 27%-42% | - 0.004 0.379 0.112 |
| DRI Low Intermediate High/very high | 78(15%) 258 (49%) 189 (36%) | 48% 36% 23% | 1.00 1.42 2.05 | 38%-58% 31%-42% 18%-29% | - 0.025 <0.001 |
1. Holtan SG, DeFor TE, Lazaryan A, Bejanyan N, Arora M, Brunstein CG, et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood. 2015;125(8):1333-8.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal