Abstract
Anti-PD-1 monoclonal antibodies have shown promising results in several hematologic malignancies. As a result, these agents are being tested in a growing number of clinical trials across multiple diseases and settings. Many participants in these trials will at some point become candidates for allogeneic hematopoietic stem cell transplant (HSCT); however, the safety and efficacy of HSCT may differ in patients previously exposed to PD-1 inhibitors given their immunomodulatory mechanism and long tissue half-life. Specifically, residual PD-1 inhibition post-HSCT could enhance allogeneic T-cell responses, which could augment the graft-vs-tumor (GVT) effect but also increase the incidence, severity or manifestations of graft-vs-host disease (GVHD) and other immune complications of HSCT.
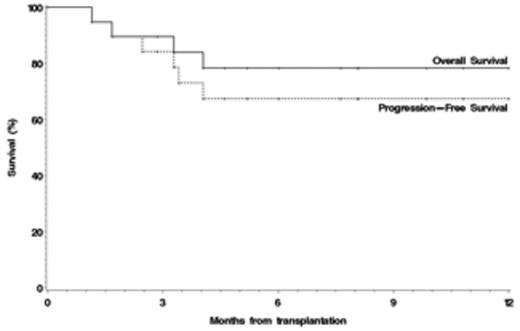
To report our experience in this setting, we retrospectively analyzed the outcomes of patients who had received a PD-1 inhibitor prior to HSCT. Between 2013 and 2015, 19 patients who previously participated in clinical trials with either pembrolizumab or nivolumab (administered in combination with ipilimumab in 1 patient) were transplanted at Brigham and Women's Hospital/Dana-Farber Cancer Institute. Median age at HSCT was 32 (range 22-67). Histologies included HL (n=11), DLBCL (n=2), FL (n=2), PMBCL (n=2), EATL (n=1), and MCL (n=1). Patients had received a median of 4 (2-8) lines of therapy prior to PD-1 blockade. 79% of patients had received a previous autologous stem cell transplant (21% as part of planned tandem procedure). Patients received a median of 8 (3-20) cycles of a PD-1 inhibitor; 74% had intervening salvage therapy between PD-1 blockade and HSCT, and transplant occurred a median of 130 (range 7-260) days after the last dose of PD-1 inhibitor. At HSCT, 63% of the patients were in CR and 16% had refractory disease. All patients received reduced intensity conditioning (RIC). 5 (26%) received marrow grafts from haploidentical sibling donors; the remaining 14 received peripheral blood stem cells, 5 from a matched sibling, 7 from a matched, 1 from a unidirectional host-versus-graft and 1 from a bidirectional mismatched unrelated donor. 3 cases of veno-occlusive disease (VOD) (16% of patients) were observed, one of them fatal. The 180-day cumulative incidences of grade 2-4 and grade 3-4 acute GVHD were 32% and 11%, respectively, and the 1-year cumulative incidence of chronic GVHD was 30%. There were 4 treatment-related deaths, (1 from VOD, 3 from severe acute GVHD occurring within 14 days of HSCT). In addition, 6 patients developed a febrile syndrome with elevated transaminases (n=3), rash (n= 4), and arthralgias (n=1) shortly after transplant, which required prolonged courses of steroids. Only 3 patients relapsed. After a median follow-up of 10 (3-23) months for survivors, the 1-year overall (OS) and progression-free survivals (PFS) were 78% (95CI, 52-91) and 67% (95CI, 41-84), respectively (Figure). The 1-year cumulative incidences of relapse and non-relapse mortality (NRM) were 11% (95CI, 2-30) and 22% (95CI, 6-43), respectively.
In conclusion, HSCT is feasible in patients previously treated with PD-1 inhibitors, with acceptable PFS and OS. Despite the heterogeneous patient population, small sample size, and limited follow-up to date, our results raise the possibility of important differences in the post-HSCT course of those patients. First, the relapse rate compares favorably to that expected for this cohort (1-year expected relapse rate based on Disease Risk Index mix 28%). Although this finding is at best suggestive given the sample size and follow-up time, it could reflect accentuation of GVT by prior PD-1 blockade. We also observed a high rate of severe complications including fatal early acute GVHD and VOD, with a higher NRM than expected in a RIC HSCT population. Furthermore, we noted the frequent occurrence of a steroid-responsive febrile syndrome. These possible effects of prior PD-1 blockade (including GVHD, VOD, febrile syndrome) did not appear related to the time from PD-1 treatment to HSCT, and were not reduced by intervening treatment before HSCT. As we accumulate experience with HSCT after PD-1 blockade, our early results may be relevant when considering the decision to proceed to HSCT and for the choice of transplantation strategies. We are presently expanding this analysis through a multi-center international collaborative study. Updated results will be presented at the meeting.
Zinzani:Celgene: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; J&J: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Gilead: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pfizer: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Takeda: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Perales:Takeda: Honoraria; Astellas: Honoraria; Amgen: Honoraria; Merck: Honoraria; NMDP: Membership on an entity's Board of Directors or advisory committees. Soiffer:Gentium SpA/Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees. Armand:Sequenta, Inc.: Research Funding; Merck: Consultancy, Research Funding; Infinity: Consultancy, Research Funding; BMS: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal