Abstract
Background:
In phase 3 studies comparing high dose melphalan (mel) with autologous stem cell transplantation (ASCT) to conventional chemotherapy, ASCT improves progression free survival (PFS) and, in some studies, overall survival (OS). However, these studies were performed before the use of potent, novel induction therapies such as bortezomib (V), lenalidomide (R), and dexamethasone. The optimal timing and benefit of ASCT in the era of novel therapies is unknown.
In our program, upon completion of stem cell harvest (SCH), some patients elect to delay ASCT after discussion of risks and benefits. The aim of this retrospective study is to compare the time to progression (TTP) and OS of patients who proceeded to ASCT early as consolidation of initial therapy, versus ASCT delayed until relapse. While data from prospective studies are eagerly awaited, this retrospective study has the advantage of a long follow up.
Methods:
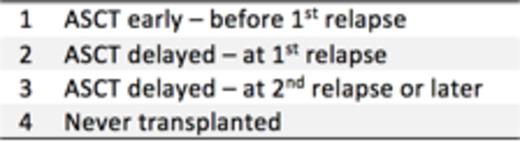
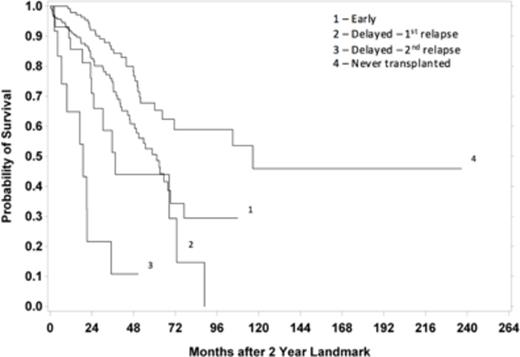
In this IRB approved, retrospective case series, electronic medical records of all patients with symptomatic MM who had SCH at Saint Vincent's Medical Center or Mount Sinai Hospital between 1/1/2005 to 6/30/2014 were reviewed. Patients were divided into the following groups:
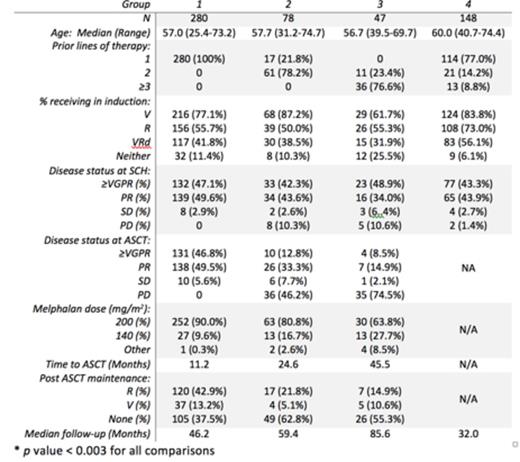
Time to progression (TTP) is calculated using Kaplan-Meier analysis. OS is calculated using a landmark analysis at 2 and 3 years after diagnosis.
Results:
572 consecutive patients were identified. 18 were excluded for incomplete data. Baseline characteristics are shown in Table 1.
The groups did not differ significantly in terms of stage (either Durie Salmon or International Staging System), disease isotype, or high risk disease features (defined by cytogenetics or FISH as amp 1q, t(14;16), t(14;20), del 17p13). The median follow-up for the entire group was 47.5 months.
Not surprisingly, the median TTP after ASCT diminished with delay of ASCT, from 28.4 mo for early ASCT to 12.2 mo for delayed (p < 0.001). That said, when comparing groups 1 and 2, there was no difference in the median time from diagnosis to progression after mel 200 mg/m2 ASCT Ð 39.1 vs 43.6 mos (p = 0.945). Using landmark analysis starting at 2 years from diagnosis, the median OS was 61.3, 37.4, 18.9, and 116.7 for groups 1, 2, 3, and 4 respectively (p = 0.087 for group 1 vs 2; p < 0.001 for group 1 vs 3; Figure 1). Landmark analysis at 3 years from diagnosis showed median OS of 50.3, 56.5, 13.9, and not reached (p = 0.41 for group 1 vs 2; p < 0.001 for group 1 vs 3).
Conclusions:
There are three findings of interest. 1) TTP in those who underwent early ASCT was 15 months longer than those who underwent ASCT at relapse. 2) TTP after SCT was comparable in groups 1 and 2, which may be attributable to the preferential use of maintenance chemo either pre or post ASCT, respectively. 3) The rank ordering of median OS by landmark analysis suggests an interplay between therapy and disease biology Ð many patients may do very well without SCT, perhaps due to durable remissions with novel regimens. The remaining groups demonstrate a striking decrease in OS as the number of relapses in a given time period increases, indicating the need for novel approaches to MM that behaves in clinically aggressive manner.
Biran:Celgene: Speakers Bureau. Jagannath:Celgene: Honoraria; Merck: Honoraria; Novartis: Honoraria; Janssen: Honoraria; Bristol Myers Squibb: Honoraria. Chari:Onyx: Consultancy, Research Funding; Millennium/Takeda: Consultancy, Research Funding; Biotest: Other: Institutional Research Funding; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Array Biopharma: Consultancy, Other: Institutional Research Funding, Research Funding; Novartis: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal