Abstract
Background: Idiopathic pneumonia syndrome (IPS) is a non-infectious pulmonary complication with diffuse lung injury that develops in 5-10% of patients who undergo hematopoietic cell transplantation (HCT) and the mortality rate remains high at 50-90%. IPS is difficult to distinguish from occult pneumonia after HCT, because it is hard to exclude all infectious etiologies. There are currently no laboratory tests to aid physicians in the early detection of IPS and other pulmonary infections. The aim of this study was to identify prognostic biomarkers of future occurrence of IPS and compare their profiles to that for subjects with infectious pneumonia.
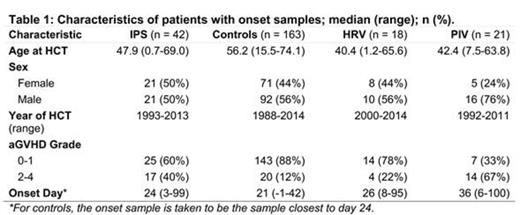
Patients and methods: Among patients transplanted between 1988 and 2014 at FHCRC, we identified 42 patients with IPS based on radiographic findings and exclusion of possible pathogens using frozen bronchoalveolar lavage (BAL) samples of occult viral infections as recently reported (Blood 2015: 24: 3789-97). HCT recipients who did not require bronchoscopic examination and who did not grow any bacterial or fungal blood cultures within 100 days after HCT were considered as controls (n=163) and samples were collected at similar timepoints as IPS cases. We examined cases of viral pneumonia confirmed by positive BAL: human rhinovirus (HRV, n=18) and parainfluenza (PIV, n=21). A set of 1129 plasma samples from pre-HCT, day 7, day 14, day 21 post-HCT and at onset of each event was analyzed. The "onset sample" for controls was the sample closest to day 24 (median day of onset for patients with pulmonary symptoms). We measured six proteins by ELISA: Suppressor of tumorigenicity 2 (ST2), tumor necrosis factor receptor 1 (TNFR1), interleukin-6 (IL-6), lymphocyte vessel endothelial receptor (LYVE)-1, endothelial protein C receptor (EPCR), and herpes virus entry mediator (HVEM). TNFR1, LYVE-1, EPCR and HVEM were discovered through a proteomics approach, and ST2 and IL-6 were also measured due to their associations with endothelial processes and IPS (Blood 2015: 15: 2435-44), respectively.
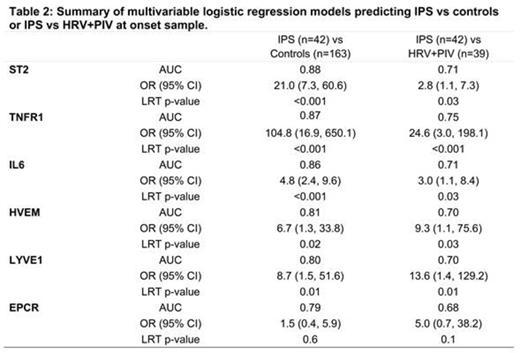
Multivariable logistic regression was used to evaluate the association of each protein with IPS vs. controls and IPS vs. HRV+PIV. Protein concentrations were log10 transformed and values below the lower limit of detection were replaced with that value (this occurred in 28% of the IL-6 measurements only). All analyses were adjusted for age, sex, transplant year, and acute GVHD status (grade 0-1 vs 2-4). Odds ratios indicate an increase in the odds of IPS for a tenfold increase in the protein concentration (Table 1). Receiver Operating Characteristic (ROC) curves were generated for each marker and if the area under the ROC (AUC) was greater than 0.7, then the analyte was considered an informative predictor of IPS.
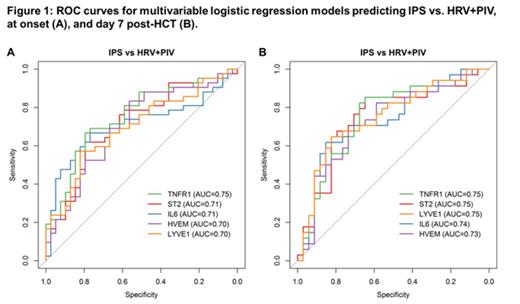
Results: Patients' characteristics are detailed in Table 1. Of the six proteins, TNFR1, ST2, LYVE-1, HVEM, and IL-6 were significantly elevated at the onset of IPS compared to controls at similar time point (adjusted, Table 2). ST2 and IL-6 were also elevated in infectious cases, although to a lesser degree. However, the biomarkers were able to distinguish IPS cases from viral infections (HRV and PIV) occurring approximately at the same time post HCT (Figure 1A). We also evaluated the prognostic value of the proteins by analyzing samples measured at day 7 post-HCT. All six proteins were elevated in IPS cases versus controls as early as day 7 with AUC from 0.85 to 0.75 (data not shown), and distinguished IPS from HRV and PIV infections (Figure 1B).
Conclusion: Five proteins, TNFR1, ST2, LYVE-, HVEM, and IL-6 were significantly elevated at the onset of respiratory failure in IPS patients as compared to patients without pulmonary injury. Although the markers were also elevated in viral pulmonary infections, they were able to distinguish IPS from HRV and PIV. Importantly, these markers were elevated as early as day 7 after HCT, prior to the clinical signs of IPS. Additional analyses combining proteins together to form a composite panel are currently ongoing.
Paczesny:Viracor laboratories: Patents & Royalties: "Methods of detection of graft-versus-host disease" (US- 13/573,766).
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal