Abstract
Introduction
The lenalidomide + dexamethasone combination (Len-dex) is an established regimen for myeloma patients (pts) with relapsed or refractory disease. In order to prolong the benefit of this effective regimen, the Myeloma Program at Princess Margaret Cancer Centre has routinely added a third agent, oral weekly cyclophosphamide (Cy), to Len-dex at the time of progression. We have now retrospectively analyzed the results of this pt cohort to assess the response rate (RR), duration of response (DOR), progression-free survival (PFS), overall survival (OS) and toxicity of the Len-dex-Cy regimen subsequent to progression on Len-dex.
Methods
The Princess Margaret Myeloma Database identified 54 patients that received Len-dex-Cy for a minimum of 4 weeks following Len-dex as a doublet between 12/2007-12/2014. Hematologic responses were assessed using modified IMWG consensus criteria. Survival times were measured in months both from the start of Len-dex and the time of addition of Cy up to date of event of interest or end of follow-up. The impact of diagnostic and clinical variables on PFS and OS were also assessed in both cases using the log rank test.
Results
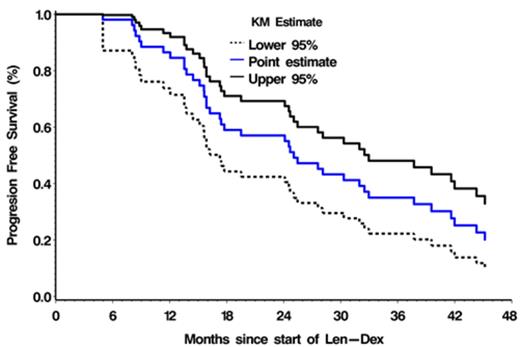
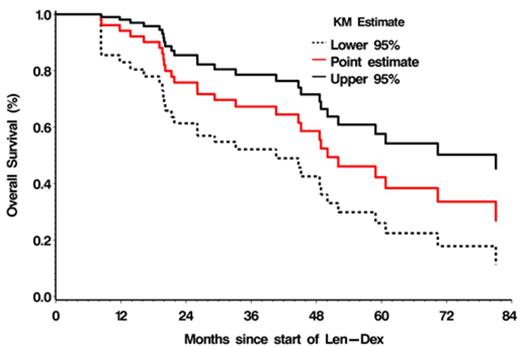
Baseline pt characteristics at addition of Cy included: median age 66 yrs; Hgb 107 g/L; creatinine 76 umol/L; albumin 36g/L; ANC 2.5 109/L; and median platelet count 158 109/L . Myeloma isotypes were IgG (61%), IgA (19%), and FLC (20%). The median number of prior regimens including Len-dex was 2; 80% pts had undergone prior ASCT. The dose of added Cy ranged between 250-500mg once weekly. Twenty-six percent patients experienced dose reductions primarily due to cytopenias. Overall, Len-dex-Cy was well tolerated with grade 3-4 toxicities in < 20% (Table 1). The mean duration of Len-Dex-Cy therapy was 8.9 months (range 0.9 - 37.7). The overall RR (≥ PR) was 41%; however clinical benefit was seen in 85% (≥ SD) pts. The median PFS was 8 months (95 % CI 5.8- 10.3 months) from addition of Cy and 25 months (95 % CI 17.3- 32.5 months) from start of Len-dex. The median OS was 24.5 months (95 % CI 15.2-41.8 months) from addition of Cy and 50.1 months (95 % CI 40.6-70.4 months) from start of Len-dex (Figure 1). Significant adverse factors for PFS were del(13q) from start of Len-dex and presence of anemia at the time of addition of Cy (p=0.027) and (p=0. 031) respectively. Decreased baseline serum albumin at the time of addition of Cy was identified as a significant factor for shorter OS (p=0.004).
Conclusions
1) The addition of Cy in pts with myeloma progressing on Len-dex resulted in a clinically meaningful extension of disease control with an acceptable safety profile; 2) The effectiveness of adding a third agent to pts with progression on a doublet regimen raises the possibility that only a limited number of resistant myeloma clone(s) is/are responsible for the progression; 3) Although subject to many limitations, the results of this sequential "on demand" approach compare favorably with our previously reported phase 2 study of the Len+ prednisone+ Cy ("CPR") regimen in which triple-drug therapy was given throughout (PFS: 25 vs 16.1 months; OS: 50.1 vs 27.6 months) (Reece et al, Br J Haematol 2015; 168: 46-54); 4) future prospective studies evaluating a strategy of adding a third agent to a doublet ( such as Len-dex) "on demand" versus using triple therapy throughout the relapse would be worthwhile; a number of potential agents, including Cy as well as other newer anti-myeloma drugs, might be candidates for such studies.
Grade 3-4 toxicities associated with Len-Dex-Cy therapy in Len-dex relapsed patients
| Toxicity . | No. of patients (%) . |
|---|---|
| Grade 3-4 Thrombocytopenia | 4 (7.7) |
| Grade 3-4 Anemia | 10 (18.8) |
| Grade 3-4 Hematuria | 1 (1.9) |
| Febrile Neutropenia | 2 (3.9) |
| Infections | 7 (12.9) |
| Secondary Malignancy | 2 (3.7) |
| Toxicity . | No. of patients (%) . |
|---|---|
| Grade 3-4 Thrombocytopenia | 4 (7.7) |
| Grade 3-4 Anemia | 10 (18.8) |
| Grade 3-4 Hematuria | 1 (1.9) |
| Febrile Neutropenia | 2 (3.9) |
| Infections | 7 (12.9) |
| Secondary Malignancy | 2 (3.7) |
| Years . | PFS Rate . | 95% Confidence Interval . | Status . | ||
|---|---|---|---|---|---|
| Lower | Upper | Events so far | Number at risk | ||
| 1 | 0.8675 | 0.74204 | 0.93454 | 7 | 45 |
| 2 | 0.5591 | 0.41457 | 0.68112 | 23 | 29 |
| 3 | 0.3433 | 0.21795 | 0.47228 | 34 | 15 |
| Years . | PFS Rate . | 95% Confidence Interval . | Status . | ||
|---|---|---|---|---|---|
| Lower | Upper | Events so far | Number at risk | ||
| 1 | 0.8675 | 0.74204 | 0.93454 | 7 | 45 |
| 2 | 0.5591 | 0.41457 | 0.68112 | 23 | 29 |
| 3 | 0.3433 | 0.21795 | 0.47228 | 34 | 15 |
| Years . | OS Rate . | 95% Confidence Interval . | Status . | ||
|---|---|---|---|---|---|
| Lower | Upper | Events so far | Number at risk | ||
| 1 | 0.9426 | 0.83250 | 0.98114 | 3 | 48 |
| 2 | 0.7428 | 0.59831 | 0.84183 | 13 | 37 |
| 5 | 0.4136 | 0.25436 | 0.56596 | 25 | 11 |
| Years . | OS Rate . | 95% Confidence Interval . | Status . | ||
|---|---|---|---|---|---|
| Lower | Upper | Events so far | Number at risk | ||
| 1 | 0.9426 | 0.83250 | 0.98114 | 3 | 48 |
| 2 | 0.7428 | 0.59831 | 0.84183 | 13 | 37 |
| 5 | 0.4136 | 0.25436 | 0.56596 | 25 | 11 |
Chen:Celgene: Consultancy, Honoraria, Research Funding. Kukreti:Celgene: Honoraria; Roche: Honoraria; Janssen Ortho: Honoraria; Amgen: Honoraria; Lundbeck: Honoraria. Tiedemann:Amgen: Honoraria; Janssen Ortho: Honoraria; Celgene: Honoraria. Prica:Celgene: Honoraria; Janssen: Honoraria. Reece:Amgen: Honoraria; Bristol-Myers Squibb: Research Funding; Lundbeck: Honoraria; Celgene: Consultancy, Honoraria, Research Funding; Janssen-Cilag: Consultancy, Honoraria, Research Funding; Merck: Research Funding; Janssen-Cilag: Consultancy, Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Onyx: Consultancy; Otsuka: Research Funding; Millennium Takeda: Research Funding; Otsuka: Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Onyx: Consultancy; Merck: Research Funding; Bristol-Myers Squibb: Research Funding; Amgen: Honoraria; Lundbeck: Honoraria; Novartis: Honoraria, Research Funding; Millennium Takeda: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal