Abstract
Background: Light chain amyloidosis (AL) is characterized by tissue deposition of misfolded proteins that cause multisystem organ dysfunction. Current treatments, including chemotherapy and autologous hematopoietic cell transplantation (AHCT), target plasma cells producing pathogenic amyloid proteins. The development of amyloid protein targeted monoclonal antibody therapy has led to an increased need for objective measurements of clinical response. The 6-minute walk test (6MWT) has been used for years as the primary outcome measure to monitor disease severity in clinical trials of heart failure (HF). For example, HF trials with cardiac devices MIRACLE (Abraham, 2002) and MUSTIC (Cazeau, 2001) demonstrated important therapeutic effects based on an improved 6MWT distance of 39 meters and a change of 23%, respectively. These findings, in conjunction with improvement in other markers of disease activity, lead to approval of cardiac resynchronization for the management of HF. Our primary objective was to determine the impact of chemotherapy on changes in 6MWT in patients with AL cardiac amyloid and correlate these changes with cardiac biomarkers.
Patients and Methods: We retrospectively analyzed outcomes of 22 AL amyloid patients with cardiac involvement. Subjects performed 6MWT at diagnosis and at the end of planned initial chemotherapy. All patients received bortezomib (B)-based chemotherapy. About half received chemotherapy alone (45%) and the others received B-based induction chemotherapy followed by AHCT (55%). To identify factors associated with changes in 6MWT, we analyzed cardiac response and changes in New York Heart Association (NYHA) class, troponin I, brain natriuretic peptide (BNP) and left ventricular ejection fraction (LV EF). Cardiac response was defined as BNP decrease of 30% or NYHA class decrease ≥ 2 in subjects with baseline NYHA class 3 or 4 (adapted from Comenzo, 2012).
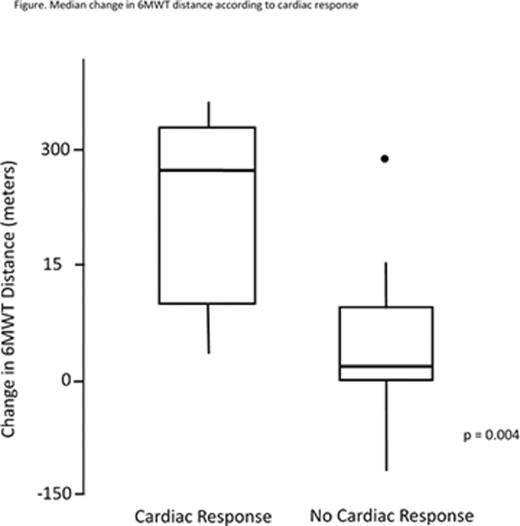
Results: At baseline, 59% (n=13) of patients were modified AL amyloid cardiac stage I/II and 41% (n=9) stage III. The median percent change in 6MWT was an increase in 26.5% with a median change of 90 meters (range, -120 to 365), p < 0.001. Overall, 81% (n=18) had improvement in 6MWT distance, 9% (n=2) declined and 9% (n=2) were unchanged. Patients had reassessment of 6MWT a median of 13.5 months from diagnosis. Hematological responses (HR) included CR (36%), VGPR (36%), PR (23%) and SD (5%). HR was not associated with change in 6MWT. Fifty percent (n=11) experienced a cardiac response. By Wilcoxon rank sum test, variables that were associated with improvement in 6MWT included improved BNP, LV EF, troponin I, NYHA class and cardiac response (all p<0.001). The median follow-up of patients was 2.15 years (range, 1.10 - 7.20).
By multivariate analysis, patients with a cardiac response had significantly better improvement in 6MWT disease compared with patients without cardiac response (p=0.02). A cardiac response was associated with a median increase of 170 meters of distance traveled by 6MWT when compared with patients having no cardiac response. All other variables tested were not statistically significant.
Conclusion: In AL amyloid patients with cardiac involvement, the 6MWT can be used as an objective marker of functional improvement complementing biochemical and imaging parameters of response. Furthermore, treatment of cardiac amyloidosis with contemporary standard regimens has a major impact on the disease process by a number of objective parameters. Patients experiencing a cardiac response had substantial improvements in 6MWT. The 6MWT should be incorporated in trials of patients with cardiac amyloid.
Cornell:Prothena: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal