Abstract

BCR-ABL transcript levels (IS%BCR-ABL) in CML patients (pts) allow to define molecular response (MR) to TKIs. MR at 3 months (M3>10%) is the strongest predictor of bad outcome and a point of divergence for changing therapy. Emerging biomarkers are being proposed in order to optimize prognosis in addition to initial MR and other clinical markers. The rate of BCR-ABL decline measured as halving time (HT) for transcript level reduction (RT0.5) at month 3 in 1GTKI (imatinib) treated pts, and the fractional clearance as a relative BCR-ABL ratio (RR3) during the first 3 months in 2GTKI (dasatinib) treated pts were recently proposed as predictive markers of outcome. Optimal responses (OR) were defined upon %ISBCR-ABL values at 3, 6 and 12 months: M3 ≤10%, M6 ≤1% y M12 ≤0,1%. Early time point prognostication could allow better outcome predictions and rapid therapeutic interventions.
Aim: to determine whether the rate of BCR-ABL decline as HT and the BCR-ABL transcripts reduction as relative ratio at M3 from baseline, have predictive value in CML pts treated with 2GTKIs.
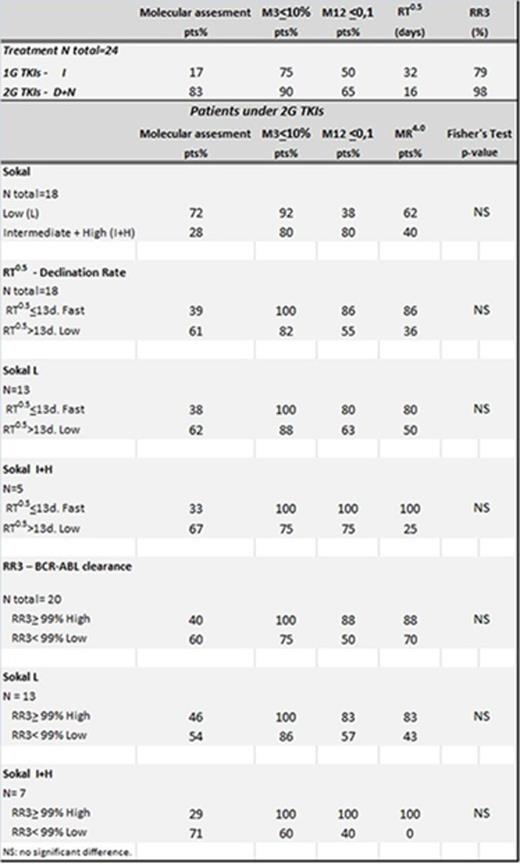
Method: BCR-ABL transcript level was measured by Q-PCR according international recommendations and results were reported as BCR-ABL/ABL on the international scale (IS BCR-ABL %). Molecular monitoring was performed prior treatment (M0) and at months 3 (M3), 6 (M6), 12 (M12) and every 6 months thereafter. RT0.5 from baseline to M3 was calculated as the time to halve by considering an exponential model of reduction during the period. The median RT0.5 and quartiles, were calculated to define rapid declines as those HT in the lowest quartile. RR3 was determined as a relative ratio of transcript clearance at M3 from baseline. The median RR3and quartiles, were considered to define high BCR-ABL clearance as those in the highest quartile. Fisher statistical test was used to determine whether the proportions of good responses were statistically different depending on the decline rate.
Results: A total of 77 CML pts were included, first line treatment: Dasatinib (D) 28%, Nilotinib (N) 32% and Imatinib (I) 40%. Sokal risk score was available in 70% pts: low (L) 67%, intermediate (In) 22% and high (H) 11%. Molecular assessment: prior therapy M0 (90%), M3 (60%), M6 (79%), M12 (78%) and M0+M3+M12(39%). Deep responses (MR4.0) were considered as IS%BCR-ABL<0,01 or no detectable transcripts in ≥10000 ABL copies. OR according to first line TKI (I vs D+N), were: M3≤10%: 75% vs 90% and M12 ≤0,1%: 50% vs 65%. RT0.5 median values for I vs D+N groups were 32d vs 16d and RR3 median values were 79% vs 98%. RT0.5 ≤13d and RR3 ≥99% were cut off values for fast responses and high clearance in pts treated with 2GTKI(83%). Milestone molecular result M3≤10% showed 20% pts with M12>0,1% and without MR4.0. All of these pts showed RT0.5 >13d and RR3 <99%. From total pts with OR, 80% pts achieved MR4.0 and all showed RR3≥99% meanwhile the remaining 20% pts who never achieved MR4.0 had RR3<99%. Higher frequencies of OR were observed in low Sokal risk pts, in RT0.5 ≤13d pts and in pts with RR3 ≥99%. High Sokal risk pts had poorer results at milestones molecular responses but those with rapid initial decline (RT0.5 ≤13d) and high BCR-ABL clearance (RR3 ≥99%) achieved molecular responses similar to those observed in the low risk sokal group.
Conclusions: Faster BCR-ABL decline and high clearance were related to OR and MR4.0 achievement in 2GTKIs patients. No direct relation between Sokal Index and M12≤ 0,1% was observed. Patients with RT0.5 ≤13d showed higher frequencies of good responses. Statistical differences were not found probably due to low sample numbers. Our data suggests that RT0.5 in 2GTKIs (N+D) patients could have a similar predictive value as reported by Branford in 2014, even though it is known that BCR-ABL measurements tend to be less satisfactory when control gene is ABL, owing to possible non-linear ratios. Whilst there were no statistical correlations probably due to the low sample number, pts with OR but no MR4.0 had low reduction rate RR3<99%. RR3>99% could provide a stronger predictive value for milestone optimal responses achievement in high risk pts. It will be necessary to extend this study including a higher number of patients treated with 2G TKIs.
Varela:Bristol Myers Squibb: Speakers Bureau; Novartis: Speakers Bureau. Moiraghi:Novartis: Speakers Bureau; Bristol Myers Squibb: Speakers Bureau. Pavlovsky:Novartis: Honoraria, Speakers Bureau; Janssen: Honoraria, Speakers Bureau. Pavlovsky:Bristol Myers Squibb: Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal