It is now widely recognized that neutrophils are highly versatile and sophisticated cells that display de novo synthetic capacity and may greatly extend their lifespan. In addition, concepts such as “neutrophil heterogeneity” and “neutrophil plasticity” have started to emerge, implying that, under pathological conditions, neutrophils may differentiate into discrete subsets defined by distinct phenotypic and functional profiles. A number of studies have shown that neutrophils act as effectors in both innate and adaptive immunoregulatory networks. In fact, once recruited into inflamed tissues, neutrophils engage into complex bidirectional interactions with macrophages, natural killer, dendritic and mesenchymal stem cells, B and T lymphocytes, or platelets. As a result of this cross-talk, mediated either by contact-dependent mechanisms or cell-derived soluble factors, neutrophils and target cells reciprocally modulate their survival and activation status. Altogether, these novel aspects of neutrophil biology have shed new light not only on the potential complex roles that neutrophils play during inflammation and immune responses, but also in the pathogenesis of several inflammatory disorders including infection, autoimmunity, and cancer.
Introduction
Over the last 2 decades, hundreds of reports have clearly documented that neutrophils are highly versatile and sophisticated cells, whose functions go far beyond the elimination of microorganisms. New fascinating aspects of typical activities, as well as novel and unanticipated functions, have been recently attributed to neutrophils. In this context, the notion that the average circulatory lifespan of neutrophils is much longer than previously thought1 and that their longevity increases several-fold during inflammation2 has changed the view under which these cells have long been considered. Accordingly, during their persistence in tissues, neutrophils can exert complex activities, including orchestration of the immune response.3,,,-7 In addition, during the late final phases of acute inflammatory responses, neutrophils become involved in the active induction of inflammation resolution through the production of proresolving lipid mediators.8 Moreover, the findings that neutrophils are also capable of reverse transmigration add another dimension to our understanding of the possible fates of these cells once they have migrated into inflamed tissues.7
Among unanticipated findings, concepts such as neutrophil heterogeneity and neutrophil plasticity have also started to emerge.9,,-12 The notion that neutrophils are able to shape the inflammatory/immune responses through de novo production of cytokines and a release of preformed proinflammatory mediators, such as proteases and alarmins, is also now well established.13 Finally, the observation that neutrophils can infiltrate lymphoid organs, including spleen and lymph nodes, as well as the demonstration that neutrophils exhibit complex cross-talk with components of the innate and adaptive immune system, which may contribute to the pathogenesis of numerous chronic inflammatory disorders, has renewed interest in these cells within the immunology community.3,,,-7
In this article, we focus on human neutrophils and summarize the recent findings on their heterogeneity and plasticity, as well as on the role that these cells play in linking the innate and adaptive arms of the immune response and in driving immune-mediated pathologies. Observations recently generated in mouse models will also be described when offering novel information on neutrophil functions.
Neutrophil heterogeneity
Evidence for the existence of neutrophil subsets with functional and phenotypic heterogeneity has recently emerged in both humans and mice.7,12 For instance, small fractions of human neutrophils have been reported to express selected molecules under both physiological and pathological conditions, including T-cell receptor-associated variable immunoreceptor,14 olfactomedin 4,12,15 neutrophil antigen B1 (NB1/CD177),12,16,17 or CD49d.18 Similarly, while senescent neutrophils express elevated levels of CXCR4, neutrophils undergoing reverse transendothelial cell migration express elevated levels of intercellular adhesion molecule-1 (ICAM-1) and low levels of CXCR1.7,12 However, the biological and functional implications of these observations remain mostly unclear.
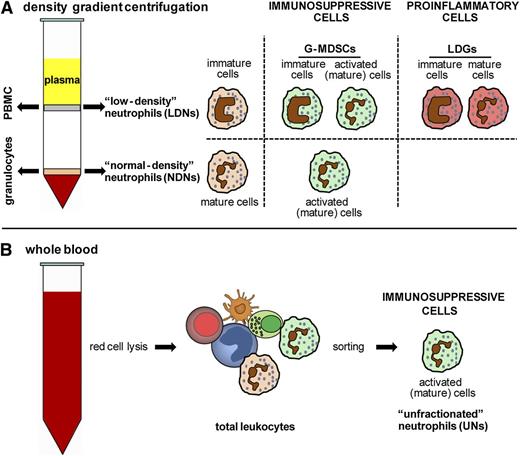
Conversely, detection of distinct circulating subsets displaying neutrophil-like morphology and showing immunosuppressive or proinflammatory functions has been well documented in systemic inflammation, autoimmune diseases, and cancer.9,-11 Some of these neutrophil populations (arbitrarily named here as low-density neutrophils [LDNs]; Figure 1A) were found to settle within the peripheral blood mononuclear cell fraction after density gradient centrifugation of the blood. Immunosuppressive subsets were also identified either within the normal density neutrophil fraction (arbitrarily named here as NDNs; Figure 1A) or within total leukocytes simply obtained by red cell lysis of whole blood (arbitrarily named here as unfractionated neutrophils [UNs]; Figure 1B). Notably, although all these neutrophil populations display a neutrophil-like morphology and the specific granulocyte marker CD66b, their phenotype, maturation/activation status, and function result differently depending on the disease type.9,-11 Such heterogeneity, particularly observed in immunosuppressive subsets, could derive, at least in part, from the fact that both immature and in vivo-activated neutrophils display altered buoyancy and sediment within the peripheral blood mononuclear cell fraction (Figure 1A). In addition, it has been recently shown that, in HIV patients, a subset of immunosuppressive neutrophils, characterized by markedly elevated levels of surface programmed death receptor 1 ligand (PDL-1), are recovered as both PDL-1high LDNs and PDL-1high NDNs after density gradient centrifugation.19 These observations would suggest that certain phenotypic/functional changes, instead of being intrinsic features of specialized neutrophil subsets, might occur in total circulating neutrophils as a result of systemic inflammation. Clearly, this issue might be solved when a careful comparison of UNs, LDNs, and NDNs from the same diseased individuals is performed.
Main neutrophil subsets identified in the peripheral blood of patients with diseases. Mature neutrophils from healthy donors, after blood centrifugation over density gradients, typically sediment on top of red cells (arbitrarily indicated as NDNs in A). By contrast, immature neutrophils, as well as mature neutrophils activated in vivo under inflammatory settings, display altered cell buoyancy properties and thus sediment within the mononuclear cell fraction (arbitrarily indicated as LDNs in A). According to the literature, LDNs may include (1) immature neutrophils found in patients with sepsis and with function mostly undefined; (2) immunosuppressive neutrophil subsets, also known as G-MDSCs, found in cancer and HIV patients or in G-CSF–treated donors and displaying either immature or activated phenotypes; and (3) proinflammatory neutrophil subsets found in patients with autoimmune diseases, recently named LDGs and consisting of a mixed population of immature and mature cells. Circulating mature neutrophil subsets, displaying immunosuppressive properties, have also been identified within either the NDN fraction in cancer and HIV patients (A) or the total leukocytes (obtained after red cell lysis of whole blood) from healthy volunteers administered with endotoxin or from patients with severe injury, cancer, or HIV infection (arbitrarily indicated as UNs in B).
Main neutrophil subsets identified in the peripheral blood of patients with diseases. Mature neutrophils from healthy donors, after blood centrifugation over density gradients, typically sediment on top of red cells (arbitrarily indicated as NDNs in A). By contrast, immature neutrophils, as well as mature neutrophils activated in vivo under inflammatory settings, display altered cell buoyancy properties and thus sediment within the mononuclear cell fraction (arbitrarily indicated as LDNs in A). According to the literature, LDNs may include (1) immature neutrophils found in patients with sepsis and with function mostly undefined; (2) immunosuppressive neutrophil subsets, also known as G-MDSCs, found in cancer and HIV patients or in G-CSF–treated donors and displaying either immature or activated phenotypes; and (3) proinflammatory neutrophil subsets found in patients with autoimmune diseases, recently named LDGs and consisting of a mixed population of immature and mature cells. Circulating mature neutrophil subsets, displaying immunosuppressive properties, have also been identified within either the NDN fraction in cancer and HIV patients (A) or the total leukocytes (obtained after red cell lysis of whole blood) from healthy volunteers administered with endotoxin or from patients with severe injury, cancer, or HIV infection (arbitrarily indicated as UNs in B).
LDN subsets
LDNs have been detected not only in patients with autoimmune disorders,11 sepsis,20 HIV infections,19,21 and cancer,10 but also in patients with graft-versus-host disease undergoing extracorporeal photopheresis treatments,22 pregnant women,23 and in healthy donors receiving granulocyte-colony-stimulating factor (G-CSF) for stem cell mobilization.24,25 LDNs described in sepsis seem to be mostly immature and functionally poorly characterized (Figure 1A).20 LDNs isolated from patients suffering from autoimmune diseases, such as systemic lupus erythematosus (SLE) and psoriasis, have been instead more recently defined as low-density granulocytes (LDGs) (Figure 1A) and mostly consist of a mixed population of immature and mature cells with neutrophil-like morphology.11 LDGs display proinflammatory functions and induce vascular damage via their enhanced ability to release inflammatory molecules and autoantigens, as well as neutrophil extracellular traps (NETs, which result from the extrusion of nuclear DNA together with antimicrobial proteins26 ).11 By contrast, LDNs identified in solid tumors, G-CSF-treated donors, and HIV patients are generally defined as granulocytic myeloid-derived suppressor cells (G-MDSCs) because of their immunosuppressive functions (Figure 1A).10,19,21,24,25 Confusion still exists regarding the phenotype of G-MDSCs, with some reports describing these cells as activated, whereas others describe them as immature cells with neutrophil-like morphology.10 The immunosuppressive function exerted by G-MDSCs is mainly defined according to their ability to suppress T-cell activation/proliferation, and it has been shown to be primarily mediated by overproduction of arginase 1 and/or reactive oxygen species (ROS).10 It should be pointed out that the relationship existing among G-MDSCs and the other identified immunosuppressive neutrophil subsets (see below) is a matter of extensive investigation in the field.9,10 Indeed, whether G-MDSCs are specialized subsets of neutrophils or originate through an altered process of granulopoiesis is still unclear.10 The recent observations that monocytic MDSCs (Mo-MDSCs) can differentiate into G-MDSCs in tumor-bearing mice and in patients with multiple myeloma27 have further complicated the scenario. It has been also suggested that splenic granulocyte and macrophage progenitors are significantly increased in patients with invasive cancer.28 The fact that freshly isolated splenic neutrophils from healthy donors were shown to inhibit the proliferation of CD4+ T cells29 raises the possibility that, similar to mice, human G-MDSCs might originate through a process of inflammation-induced extramedullary granulopoiesis.
Other neutrophil immunosuppressive subsets
To date, several NDNs inhibiting T-cell proliferation through diverse mechanisms have been identified (Figure 1A), including the CD15+CD16low and the CCL2-producing subsets detected in cancer patients30,31 and the PDL-1high subset detected in HIV patients.19 The presence of immunosuppressive UNs has been instead reported in healthy volunteers administered with endotoxin or in patients with severe injury,32,33 cancer,34 giant-cell arteritis under glucocorticoid treatment,35 and HIV-1 infection19 (Figure 1B). However, at least to our knowledge, only Pillay et al32 have formally sorted a subset of activated (CD16brightCD62Ldim) mature neutrophils from total leukocytes and shown it to effectively inhibit T-cell responses through macrophage-1 antigen (Mac-1)- and ROS-dependent mechanisms.32
Neutrophil plasticity
The concept that neutrophils may display a previously unanticipated plasticity derives from observations on their ability, under inflammatory settings, to differentiate into other myeloid cell types. Accordingly, the fact that neutrophils can acquire antigen presenting (APC)-like properties and dendritic cell (DC) characteristics on long-term incubation with discrete cytokine combinations, or be reprogrammed into macrophages, has been known for a long time.3,,-6,36 More recently, both immature and mature mouse neutrophils have been shown to differentiate into hybrid populations showing dual phenotypes and properties of both neutrophils and DCs, either when cultured in vitro with granulocyte macrophage-colony-stimulating factor (GM-CSF) or when transferred to inflammatory settings in vivo.37 This study has been corroborated in humans, in whom purified bone marrow-derived neutrophils were demonstrated to differentiate into a hybrid population characterized by the expression of both neutrophil and DC markers on in vitro treatment with GM-CSF, tumor necrosis factor-α (TNFα), and interleukin-4 (IL-4) for 7 days.37 Further depicting their extraordinary plasticity, a very small fraction of neutrophils has been shown to survive in vitro without the addition of exogenous cytokines or growth factors and, after 7 days of culture, ultimately transform into giant phagocytic cells.38 However, the potential significance of these giant neutrophils to inflammatory/anti-inflammatory processes in vivo remains to be elucidated. In this context, it is plausible that with the development of very efficient cell isolation techniques and the increased availability of neutrophils purified from various compartments, such as spleen, peritoneal exudates, lungs, oral cavity, skin, bone marrow, cord blood, and placenta, other neutrophil subpopulations with specialized functions will be discovered.
Neutrophil-centered cross-talk
It has been demonstrated that human neutrophils, other than interacting with nonimmune cell types such as platelets39 and mesenchimal stem cells,3 can establish, in vitro and in vivo, cross-talk with innate immune cells, such as DCs, monocytes, macrophages, and natural killer (NK) cells, as well as with adaptive immune cells, such as T and B cells, or related subpopulations3,,-6 (summarized in Tables 1 and 2). As highlighted below, by establishing such bidirectional interactions, neutrophils receive signals modulating their survival and effector functions on the one hand, whereas they initiate, amplify, and/or suppress innate or adaptive immune effector responses on the other hand. Studies made in a variety of experimental animal models (listed in supplemental Tables 1 and 2 on the Blood Web site) not only have corroborated the existence of neutrophil-centered cross-talk, but have also highlighted their pathophysiological significance.
Cross-talk between human neutrophils and innate immune cells
| Neutrophil cross-talk with . | Cross-talk outcome . | References . |
|---|---|---|
| DCs: moDCs | Reduced CD40, CD80, and CD86 expression, and decreased ability to stimulate T cell proliferation in modcs engulfing apoptotic and/or necrotic neutrophils | 1 |
| Enhancement, by fMLF-, TNFα- or LPS-activated neutrophils, of moDC maturation and ability to promote T cell proliferation and Th1 polarization, via Mac-1/DC-SIGN and/or Mac-1/CEACAM1 interactions and TNFα release | 2-3 | |
| Enhancement, by apoptotic and/or live neutrophils, of moDC maturation and ability to promote T cell proliferation, via CD18-mediated contact dependent mechanisms and release of soluble factors | 4 | |
| Inhibition, by non-infected apoptotic neutrophils, of M tuberculosis-induced moDC maturation and ability to induce lymphocyte proliferation. Enhancement of moDC ability to drive lymphocyte proliferation by M tuberculosis-induced apoptotic neutrophils | 5 | |
| Promotion of CD4+FOXP3+ Treg differentiation by moDCs treated with neutrophil-derived elastase | 6-7 | |
| Inhibition, by neutrophil-derived EVs, of moDC maturation and capacity to induce T cell proliferation | 8 | |
| Enhancement, by BCG-infected neutrophils, of moDC maturation and ability to recall reactivity of T cells isolated from vaccinated donors, via cell-contact dependent mechanisms | 9 | |
| Modulation of DC functions by neutrophil-derived alarmins (defensins, cathelicidin, lactoferrin and high-mobility group box-1 protein) | Reviewed in Dumitru et al10 | |
| moDC internalization and cross-presentation of antigens previously processed by neutrophils | 11 | |
| Inhibition of moDC maturation and cytokine production by neutrophil-derived myeloperoxidase | 12 | |
| pDCs | Enhancement of pDC-derived IFNα by NETs released by SLE neutrophils containing self-DNA in complex with antimicrobial peptides | 13-14 |
| Enhancement of pDC-derived IFNα by NETs containing DNA complexed with secretory leukocyte protease inhibitor and neutrophil elastase or cathepsin G | 15-16 | |
| slanDCs | Enhancement, by neutrophils, of slanDC-derived IL-12p70, via CD18/ICAM-1 interactions | 17 |
| Enhancement of neutrophil and slanDC survival by reciprocal interactions occurring through contact-dependent mechanisms | 18 | |
| Macrophages | Inhibition of proinflammatory cytokine production in macrophages engulfing apoptotic neutrophils | Reviewed in Bowers et al19 |
| Inhibition of macrophage activation, cytokine production and phagocytosis by neutrophil-derived EVs | 20-21 | |
| Enhancement of macrophage antimicrobial activity by the uptake of antimicrobial peptides from neutrophils | Reviewed in Rieber et al22 | |
| Enhancement of macrophage phagocytosis and reactive oxygen species (ROS) production by neutrophil-derived primary granule proteins | 23-24 | |
| Enhancement of macrophage-derived cytokines by M tuberculosis-induced NETs | 25 | |
| Activation of NLRP3 inflammasome and induction of IL-1β and IL-18 release in macrophages by NETs from LPS-activated neutrophils or resting LDGs from SLE patients | 26 | |
| Enhancement, by PMA-induced NETs, of cytokine production in LPS-stimulated macrophages. Clearance of PMA-induced NETs by resting macrophages | 27 | |
| NK cells | Modulation, by NK cells, of neutrophil survival, activation and HB-EGF release, via GM-CSF, IFNγ and TNFα release as well as contact-dependent mechanisms | 28-29 |
| Enhancement, by neutrophils, of NK-derived IFNγ, via ICAM-3 and CD11d/CD18 interactions | 17,30 | |
| Modulation of NK cell functions by neutrophil-derived molecules, such as arginase-1, serine proteases, defensins and ROS | Reviewed in Tsuda et al31 | |
| Impairment of NK cell maturation and functions in neutropenic patients, additionally supported by in vivo experimental models | 32 | |
| Induction, by NK cells, of caspase-dependent neutrophil apoptosis, via NKp46- and Fas-dependent mechanisms | 33 | |
| Enhancement, by NK cells, of neutrophil antifungal activity. Inhibition of NK cell activation by neutrophils in the presence of Candida albicans | 34 | |
| Inhibition of pro-inflammatory, and enhancement of anti-inflammatory, cytokine production in NK cells, by neutrophil–derived EVs | 35 | |
| Induction, by NK cells, of apoptosis in galactosaminogalactan (GG)-treated neutrophils, via NKG2D mediated interactions | 36 | |
| ILCs | Enhancement of neutrophil B-cell helper functions by splenic ILCs, via GM-CSF | 37 |
| Neutrophil cross-talk with . | Cross-talk outcome . | References . |
|---|---|---|
| DCs: moDCs | Reduced CD40, CD80, and CD86 expression, and decreased ability to stimulate T cell proliferation in modcs engulfing apoptotic and/or necrotic neutrophils | 1 |
| Enhancement, by fMLF-, TNFα- or LPS-activated neutrophils, of moDC maturation and ability to promote T cell proliferation and Th1 polarization, via Mac-1/DC-SIGN and/or Mac-1/CEACAM1 interactions and TNFα release | 2-3 | |
| Enhancement, by apoptotic and/or live neutrophils, of moDC maturation and ability to promote T cell proliferation, via CD18-mediated contact dependent mechanisms and release of soluble factors | 4 | |
| Inhibition, by non-infected apoptotic neutrophils, of M tuberculosis-induced moDC maturation and ability to induce lymphocyte proliferation. Enhancement of moDC ability to drive lymphocyte proliferation by M tuberculosis-induced apoptotic neutrophils | 5 | |
| Promotion of CD4+FOXP3+ Treg differentiation by moDCs treated with neutrophil-derived elastase | 6-7 | |
| Inhibition, by neutrophil-derived EVs, of moDC maturation and capacity to induce T cell proliferation | 8 | |
| Enhancement, by BCG-infected neutrophils, of moDC maturation and ability to recall reactivity of T cells isolated from vaccinated donors, via cell-contact dependent mechanisms | 9 | |
| Modulation of DC functions by neutrophil-derived alarmins (defensins, cathelicidin, lactoferrin and high-mobility group box-1 protein) | Reviewed in Dumitru et al10 | |
| moDC internalization and cross-presentation of antigens previously processed by neutrophils | 11 | |
| Inhibition of moDC maturation and cytokine production by neutrophil-derived myeloperoxidase | 12 | |
| pDCs | Enhancement of pDC-derived IFNα by NETs released by SLE neutrophils containing self-DNA in complex with antimicrobial peptides | 13-14 |
| Enhancement of pDC-derived IFNα by NETs containing DNA complexed with secretory leukocyte protease inhibitor and neutrophil elastase or cathepsin G | 15-16 | |
| slanDCs | Enhancement, by neutrophils, of slanDC-derived IL-12p70, via CD18/ICAM-1 interactions | 17 |
| Enhancement of neutrophil and slanDC survival by reciprocal interactions occurring through contact-dependent mechanisms | 18 | |
| Macrophages | Inhibition of proinflammatory cytokine production in macrophages engulfing apoptotic neutrophils | Reviewed in Bowers et al19 |
| Inhibition of macrophage activation, cytokine production and phagocytosis by neutrophil-derived EVs | 20-21 | |
| Enhancement of macrophage antimicrobial activity by the uptake of antimicrobial peptides from neutrophils | Reviewed in Rieber et al22 | |
| Enhancement of macrophage phagocytosis and reactive oxygen species (ROS) production by neutrophil-derived primary granule proteins | 23-24 | |
| Enhancement of macrophage-derived cytokines by M tuberculosis-induced NETs | 25 | |
| Activation of NLRP3 inflammasome and induction of IL-1β and IL-18 release in macrophages by NETs from LPS-activated neutrophils or resting LDGs from SLE patients | 26 | |
| Enhancement, by PMA-induced NETs, of cytokine production in LPS-stimulated macrophages. Clearance of PMA-induced NETs by resting macrophages | 27 | |
| NK cells | Modulation, by NK cells, of neutrophil survival, activation and HB-EGF release, via GM-CSF, IFNγ and TNFα release as well as contact-dependent mechanisms | 28-29 |
| Enhancement, by neutrophils, of NK-derived IFNγ, via ICAM-3 and CD11d/CD18 interactions | 17,30 | |
| Modulation of NK cell functions by neutrophil-derived molecules, such as arginase-1, serine proteases, defensins and ROS | Reviewed in Tsuda et al31 | |
| Impairment of NK cell maturation and functions in neutropenic patients, additionally supported by in vivo experimental models | 32 | |
| Induction, by NK cells, of caspase-dependent neutrophil apoptosis, via NKp46- and Fas-dependent mechanisms | 33 | |
| Enhancement, by NK cells, of neutrophil antifungal activity. Inhibition of NK cell activation by neutrophils in the presence of Candida albicans | 34 | |
| Inhibition of pro-inflammatory, and enhancement of anti-inflammatory, cytokine production in NK cells, by neutrophil–derived EVs | 35 | |
| Induction, by NK cells, of apoptosis in galactosaminogalactan (GG)-treated neutrophils, via NKG2D mediated interactions | 36 | |
| ILCs | Enhancement of neutrophil B-cell helper functions by splenic ILCs, via GM-CSF | 37 |
References to Table 1 are listed in the supplemental Materials.
Cross-talk between human neutrophils and adaptive immune cells
| Neutrophil cross-talk with . | Cross-talk outcome . | References . |
|---|---|---|
| T cells: CD4+ and/ or CD8+ T cells | Induction, by antigen-pulsed neutrophils, of lymphocyte proliferation in a non-MHC-restricted fashion | 1 |
| Induction of antigen specific T cell activation by neutrophil precursors that have acquired DC-like properties after treatment with GM-CSF, IL-4 and TNFα | 2 | |
| MHC class II-restricted antigen presentation to T cells by GM-CSF plus IFNγ-treated neutrophils | 3-4 | |
| Enhancement of T cell proliferation by neutrophils from patients with Staphylococcus aureus infections | 5 | |
| Cross-presentation, by neutrophils, of soluble antigens to CD8+T cells | 6 | |
| Neutrophil and T cell reciprocal modulation of lifespan and function, via cytokine release and/or cell-contact dependent mechanisms | Reviewed in Kolaczkowska and Kubes7 | |
| Enhancement of neutrophil survival and activation by anti-CD3-activated CD4+T and, more potently, CD8+T cells, via TNFα, IFNγ and GM-CSF release | 8 | |
| Recruitment of Th1 and Th17, but not Th2, cells by neutrophils. Enhancement of neutrophil recruitment, survival and activation by Th17 cells, mostly via CXCL8/IL-8 and GM-CSF release, respectively | 9 | |
| Reduction of viability, activation and proliferation of CD4+T cells by unstimulated neutrophils | 10 | |
| Inhibition of T cell activation, proliferation and function by activated neutrophils, via release of arginase-1, production of ROS and/or cell-contact dependent mechanisms | 11-13 | |
| Inhibition of CD4+T cell activation and proliferation by splenic neutrophils | 14 | |
| Inhibition of T cell activation and proliferation by CD11cbright/CD62Ldim/CD11bbright/CD16bright neutrophils isolated from individuals injected with endotoxin, via Mac-1-, ROS- and/or PDL-1 (B7-H1)- dependent mechanisms | 15-16 | |
| Inhibition of T cell activation and proliferation by activated mature neutrophils or granulocytic myeloid-derived suppressor cells (G-MDSCs) from cancer patients, mainly via arginase-1 and ROS overproduction | Reviewed in Wang et al17 | |
| Priming of T cell responses to specific antigens by NETs | 18 | |
| Tregs | Recruitment of neutrophils by Tregs, via CXCL8/IL-8 release | 19 |
| Promotion of CD4+FOXP3+ Treg differentiation by moDCs treated with neutrophil-derived elastase | 20-21 | |
| γδ T cells | Killing of LPS-treated neutrophils by γδ T cells, via contact dependent mechanisms mediated by surface heat shock protein-72 | 22 |
| Enhancement of neutrophil migration, phagocytosis and α-defensin release by zoledronic acid-activated γδ T cells, via release of soluble factors | 23 | |
| Enhancement of neutrophil survival and activation by phosphoantigen activated-γδ T cells. Activation of γδ T cells by neutrophils harboring phagocytosed bacteria | 24 | |
| Suppression of spontaneous and phosphoantigen-induced activation in γδ T cells by neutrophils, via ROS production | 25 | |
| Inhibition of zoledronate-mediated Vγ9Vδ2 T cell activation by neutrophils, via hydrogen peroxide, serine proteases and arginase-1 release | 26 | |
| Enhancement of the migration, survival and proliferation of tumor infiltrated G-MDSCs by activated γδ T isolated from tumor tissues | 27 | |
| iNKT cells | Inhibition of iNKT-derived IFNγ and iNKT cytotoxicity by neutrophils, via contact dependent mechanisms | 28 |
| B cells | Enhancement of B cell survival and proliferation by G-CSF-or antineutrophil cytoplasmic antibody (ANCA)-stimulated neutrophils, via BAFF production | 29-30 |
| Enhancement of plasma cell survival by neutrophils, via APRIL secretion | 31 | |
| Induction of immunoglobulin (Ig) class switching, somatic hypermutation and antibody production in MZ B cells by splenic neutrophils, via BAFF, APRIL and IL-21 production | 14 |
| Neutrophil cross-talk with . | Cross-talk outcome . | References . |
|---|---|---|
| T cells: CD4+ and/ or CD8+ T cells | Induction, by antigen-pulsed neutrophils, of lymphocyte proliferation in a non-MHC-restricted fashion | 1 |
| Induction of antigen specific T cell activation by neutrophil precursors that have acquired DC-like properties after treatment with GM-CSF, IL-4 and TNFα | 2 | |
| MHC class II-restricted antigen presentation to T cells by GM-CSF plus IFNγ-treated neutrophils | 3-4 | |
| Enhancement of T cell proliferation by neutrophils from patients with Staphylococcus aureus infections | 5 | |
| Cross-presentation, by neutrophils, of soluble antigens to CD8+T cells | 6 | |
| Neutrophil and T cell reciprocal modulation of lifespan and function, via cytokine release and/or cell-contact dependent mechanisms | Reviewed in Kolaczkowska and Kubes7 | |
| Enhancement of neutrophil survival and activation by anti-CD3-activated CD4+T and, more potently, CD8+T cells, via TNFα, IFNγ and GM-CSF release | 8 | |
| Recruitment of Th1 and Th17, but not Th2, cells by neutrophils. Enhancement of neutrophil recruitment, survival and activation by Th17 cells, mostly via CXCL8/IL-8 and GM-CSF release, respectively | 9 | |
| Reduction of viability, activation and proliferation of CD4+T cells by unstimulated neutrophils | 10 | |
| Inhibition of T cell activation, proliferation and function by activated neutrophils, via release of arginase-1, production of ROS and/or cell-contact dependent mechanisms | 11-13 | |
| Inhibition of CD4+T cell activation and proliferation by splenic neutrophils | 14 | |
| Inhibition of T cell activation and proliferation by CD11cbright/CD62Ldim/CD11bbright/CD16bright neutrophils isolated from individuals injected with endotoxin, via Mac-1-, ROS- and/or PDL-1 (B7-H1)- dependent mechanisms | 15-16 | |
| Inhibition of T cell activation and proliferation by activated mature neutrophils or granulocytic myeloid-derived suppressor cells (G-MDSCs) from cancer patients, mainly via arginase-1 and ROS overproduction | Reviewed in Wang et al17 | |
| Priming of T cell responses to specific antigens by NETs | 18 | |
| Tregs | Recruitment of neutrophils by Tregs, via CXCL8/IL-8 release | 19 |
| Promotion of CD4+FOXP3+ Treg differentiation by moDCs treated with neutrophil-derived elastase | 20-21 | |
| γδ T cells | Killing of LPS-treated neutrophils by γδ T cells, via contact dependent mechanisms mediated by surface heat shock protein-72 | 22 |
| Enhancement of neutrophil migration, phagocytosis and α-defensin release by zoledronic acid-activated γδ T cells, via release of soluble factors | 23 | |
| Enhancement of neutrophil survival and activation by phosphoantigen activated-γδ T cells. Activation of γδ T cells by neutrophils harboring phagocytosed bacteria | 24 | |
| Suppression of spontaneous and phosphoantigen-induced activation in γδ T cells by neutrophils, via ROS production | 25 | |
| Inhibition of zoledronate-mediated Vγ9Vδ2 T cell activation by neutrophils, via hydrogen peroxide, serine proteases and arginase-1 release | 26 | |
| Enhancement of the migration, survival and proliferation of tumor infiltrated G-MDSCs by activated γδ T isolated from tumor tissues | 27 | |
| iNKT cells | Inhibition of iNKT-derived IFNγ and iNKT cytotoxicity by neutrophils, via contact dependent mechanisms | 28 |
| B cells | Enhancement of B cell survival and proliferation by G-CSF-or antineutrophil cytoplasmic antibody (ANCA)-stimulated neutrophils, via BAFF production | 29-30 |
| Enhancement of plasma cell survival by neutrophils, via APRIL secretion | 31 | |
| Induction of immunoglobulin (Ig) class switching, somatic hypermutation and antibody production in MZ B cells by splenic neutrophils, via BAFF, APRIL and IL-21 production | 14 |
iNKT, invariant NKT cells.
References to Table 2 are listed in the supplemental Materials.
Cross-talk between neutrophils and innate immune cells
Neutrophils and DCs.
Neutrophils can modulate, either positively or negatively, the survival, maturation status, and functions of monocyte-derived DCs (moDCs), 6-sulfo LacNAc+ DCs (slanDCs), and plasmacytoid DCs (pDCs) (Table 1; supplemental Table 1).3,5,6,40 Survival and other effector activities of neutrophils can be modulated by DCs in a reciprocal manner, as for instance demonstrated to occur under neutrophil/slanDC coculture conditions (Table 1). Neutrophil-DC cross-talk is regulated either by contact-dependent mechanisms or via the release of cell-derived products, such as cytokines, inflammatory mediators, and, in the case of neutrophils, extracellular vesicles (EVs, also known as microparticles or ectosomes).3 EVs are cell-derived membrane vesicles of heterogeneous size, containing hundreds of distinct proteins, lipids, and microRNAs,41 that have been shown to mainly down-modulate the inflammatory responses in activated DCs (Table 1). In this context, recent publications have reported that NETs can also mediate cross-talk between neutrophils and several DC subsets and suggested that they represent a novel mechanism involved in the pathogenesis of SLE42,43 and psoriasis in humans,44,45 or type 1 diabetes (T1D)46 and autoimmune vasculitis47 in mice. Interestingly, inhibitory effects of NETs on lipopolysaccharide (LPS)-induced DC maturation and cytokine production have also been observed, given that NET-treated DCs inhibit T-lymphocyte proliferation and skew T-cell differentiation toward a T-helper type 2 (Th2) phenotype (L. S. Barrientos, V. Marin-Esteban, and S. Chollet-Martin, unpublished data, 2014). Likewise, myeloperoxidase release by neutrophils has recently been identified as another manner through which DC activation and function can be negatively modulated.48
Neutrophils and macrophages.
Neutrophils may positively modulate cytokine production and microbicidal activity in macrophages49 (Table 1; supplemental Table 1), for instance, via NET release, as observed in models using human neutrophils isolated from SLE patients or activated in vitro with LPS or Mycobacterium tuberculosis (Table 1). Human neutrophils may also inhibit macrophage activation and/or macrophage-derived TNFα and CXCL8 by either efferocytosis-dependent mechanisms or EV release (Table 1).
Neutrophils and NK cells.
It has been widely documented that activated NK cells secrete multiple cytokines (including GM-CSF, interferon-γ [IFNγ], and TNFα) able to influence the activation status of neutrophils under coculture conditions, by extending their lifespan, by up-regulating their expression of activation markers, and by potentiating their capacity to phagocytose, to produce ROS, and to synthesize heparin binding-epidermal growth factor (HB-EGF) (Table 1; supplemental Table 1).3,50 Evidence that NK cells may instead induce neutrophil apoptosis under specific coculture conditions, either via NKp46- and Fas-dependent mechanisms or via interactions between NKG2D and MHC class I chain-related molecule A, also exist in the literature (Table 1). Reciprocally, neutrophils modulate NK cell survival, proliferation, cytotoxic activity and production of IFNγ, via the generation of prostaglandins or ROS, through release of granule components or via contact-dependent mechanisms (Table 1).3,50 In addition, recent observations suggest that, by releasing EVs, neutrophils negatively modulate NK cell functions, in particular skewing NK-derived cytokines from a proinflammatory to an anti-inflammatory profile.51 The relevance of the in vitro findings on cross-talk between human neutrophils and NK cells has been highlighted by studies proving that, under steady state, neutrophils are crucial for NK-cell development in both humans and mice.52 Additional evidence that cross-talk between these 2 cell types can also occur in vivo has recently been shown in a mouse model of systemic fungal infection, in which an IL-17-NK cell-GM-CSF axis was found to be critical for the modulation of neutrophil fungicidal activity.53 In line with these findings, in vitro coculture of human NK cells and neutrophils in the presence of Candida albicans resulted in a NK-mediated enhancement of neutrophil antifungal activity, concomitantly with a neutrophil-mediated inhibition of NK-cell activation,54 suggesting that interactions between these 2 cell types might serve to reciprocally modulate their responses.
Neutrophils and innate lymphoid cell types.
Mucosal tissues contain a large number of innate lymphocytes now collectively referred to as innate lymphoid cells (ILCs).55 Evidence has been emerging that the various ILC subsets play a key role in the orchestration of immunity to infection and in the pathogenesis of allergic and autoimmune diseases.55 In this context, a recently described human splenic ILC subset, with mucosa-like properties, has been found to activate marginal zone (MZ) B cells, either directly via B cell-activating factor (BAFF), CD40 ligand, and Delta-like 1 production, or indirectly by producing GM-CSF.56 The latter cytokine, in turn, has been shown to potentiate the ability of splenic neutrophils to directly activate B-cell functions.56 It is likely that additional cross-talk between neutrophils and other ILC subsets will be soon uncovered.
Cross-talk between neutrophils and adaptive immune cells
Neutrophils and B cells.
Neutrophils can modulate B-cell functions (Table 2; supplemental Table 2) in part through the production of cytokines crucial for B-cell survival, maturation, and differentiation, such as BAFF and a proliferation-inducing ligand (APRIL).57 The concept that human neutrophils can function as B-cell helpers has emerged by the demonstration that freshly isolated splenic neutrophils induce a T cell-independent antibody response by MZ B cells, via BAFF, APRIL, and IL-21 release.29 Intriguingly, B-cell helper functions by splenic neutrophils have not been reproduced by other groups,58 likely due to differences in the protocol used to collect, store, and process the splenic tissue and/or in the purity/manipulation of the neutrophil or B-cell populations, as pointed out by the same authors.58 Conversely, recent in vivo data confirm that splenic mouse neutrophils support preimmune immunoglobulin (Ig)G3 production, as well as postimmune IgM, IgG2b, IgG2c, and IgG3 responses to repetitive immunization with polysaccharides such as 2,4,6-trinitrophenyl-ficoll (A. Chorny and A. Cerutti, unpublished data, 2014). Neutrophils have also been proposed to play a role in the pathogenesis of B-cell lymphomas, either through the production of APRIL59 or, based on studies in mice, through NET release60 (supplemental Table 2).
Neutrophils and T cells.
The ability of both naïve/polarized T cells and neutrophils to reciprocally influence their effector functions under coculture conditions, either via chemokine and cytokine production or contact-dependent mechanisms, have been extensively discussed in previous reviews3,5,6,61 (Table 2; supplemental Table 2). Earlier studies, however, had already uncovered that T cell-derived cytokines, particularly IFNγ, GM-CSF, and TNFα, function as priming agents for human neutrophils, namely as factors able to greatly enhance neutrophil responsiveness on secondary stimulation.62 A variety of fast neutrophil responses involved in inflammatory and immune processes may be primed, ultimately leading to increased oxidative metabolism (eg, ROS production), degranulation, surface receptor expression, phagocytosis, and cytotoxicity.62,63 At the molecular level, neutrophil priming by T cell-derived cytokines may occur through multiple, but not yet completely identified, mechanisms, including de novo gene induction, post-translational modifications of specific effector proteins, and/or modification of signaling pathways.62,63 Neutrophil-T cell bidirectional interactions are, in turn, supported by original reports suggesting that humans and mouse neutrophils can positively modulate T-cell functions, either indirectly, via DC activation, or directly, through chemokine/cytokine production, APC-like properties, or NET-mediated mechanisms.3,-5 However, because several studies also suggest that, as described above, activated neutrophils or neutrophil subsets have a predominantly suppressive function on T cells,9,10 it is clear that the outcome of neutrophil-T cell cross-talk is a function of the experimental settings during which these interactions occur (Table 2; supplemental Table 2).
Controversial observations are emerging on the cross-talk occurring between human neutrophils and γδ T cells. Although initial evidence suggested that γδ T cells are involved in neutrophil killing to limit host tissue damage during sepsis, more recent studies report that γδ T cells positively modulate neutrophil recruitment, activation, and survival (Table 2; supplemental Table 2). Similarly, although human neutrophils were initially shown to stimulate γδ T cells,64 more recent evidence suggests that neutrophils may, mostly via ROS production, negatively modulate spontaneous and phosphoantigen-induced γδ T-cell activation65 or contribute to the loss of peripheral blood Vγ9Vδ2 T cells observed after long-term or high-dose administration of zoledronate.66 Considering that the stimulatory functions of neutrophils on γδ T cells were reported to occur only in the presence of autologous monocytes,64 it is plausible that technical differences, intrinsic to the experimental conditions used, might influence the resulting neutrophil-γδ T-cell interactions. Very recently, human γδ T cells have also shown to contribute to the recruitment, survival, and proliferation of tumor-infiltrated G-MDCs in colorectal cancer, through the release of IL-17A, CXCL8, GM-CSF, and TNFα.67 Strikingly, it has been recently observed that unconventional T cells, including γδ T cells and mucosal-associated invariant T cells, induce neutrophils to acquire a unique activated phenotype with APC properties not only for CD4+ but also for CD8+ T cells (M. S. Davey, B. Moser, and M. Eberl, unpublished data, 2014).
Finally, neutrophils have been shown to impair iNKT-cell function, in both mice and humans, through cell-cell contact-dependent mechanisms (Table 2; supplemental Table 2).
Neutrophils in diseases
Most of our knowledge on neutrophil functions in human diseases derives from correlative studies on cells isolated from patients. However, because the isolation procedures, cell purity, or drug treatment these patients are receiving often limit the reliability of the observations made, the role of neutrophils in disease pathogenesis is mostly extrapolated from studies in experimental animal models. In this context, remarkable improvements have been made in developing tools suitable for studying the immunoregulatory role of neutrophils in vivo, including the availability of neutrophil-specific depleting antibodies (such as the anti-Ly6G/1A8 monoclonal antibody), the generation of mice carrying the conditional deletion of the loxP-flanked allele of interest under the control of neutrophil-specific promoters, as well as of humanized mice carrying functional human neutrophils. In any case, crucial neutrophil functions in humans, such as their indispensable role in providing protection against bacterial and fungal infections have been substantiated by studying patients affected by genetically determined neutrophil disorders.68 In this context, novel mutations causing neutrophil defects, specifically in genes enconding caspase recruitment domain-containing protein 9,69 IFN-stimulated gene 15,70 vacuolar protein sorting 45,71 and syntaxin–binding protein 272 have been recently identified. For instance, the lack of Mycobacterium-induced secretion of INF-stimulated gene 15, an IFNα/β-inducible ubiquitin-like intracellular protein, mostly by neutrophils, determined a reduced ability of lymphocytes and, especially, NK cells, to produce IFNγ, pointing for a novel player involved in the neutrophil-NK cell cross-talk for optimal antimycobacterial immunity.70
A growing amount of evidence suggests that neutrophils play critical roles in chronic inflammatory conditions, such as atherosclerosis, type 2 diabetes, vascular, liver, and intestinal inflammation, and local and systemic allergic reactions.5,-7,73,74 Herein, we focus on recent discoveries concerning novel neutrophil functions in infection, autoimmunity, and cancer.
Neutrophils in infection
The importance of neutrophils in host defense and infectious diseases has been underscored by recent discoveries demonstrating that their function is essential in combating intracellular bacteria (such as mycobacteria or Brucella abortus),5,75 parasites,5,76,77 and pathogenic viruses (such as human immunodeficiency virus-1 or influenza virus).78,79 The latter data are further supported by the documentation that, in addition to Toll-like receptors (TLRs), C-type lectin receptors,80,81 and inflammasome components,82 neutrophils also express cytoplasmic sensors. The latter include receptors recognizing pathogen-derived intracellular RNA, such as retinoic acid inducible-I and melanoma differentiation-associated antigen 5, and receptors recognizing pathogen-derived intracellular DNA, such as IFN-inducible protein 16, leucine-rich repeat in Flightless I interacting protein-1, DEAD (Asp-Glu-Ala-Asp) box polypeptide 41, or stimulator of interferon genes.83 In such regard, the description of surface TLR9 in neutrophils points for additional mechanisms whereby neutrophils could sense microbial-derived hypomethylated CpG DNA.84 Similarly, TLR4, the receptor for LPS, was shown to function, in neutrophils, also as receptor for shiga toxin,85 which is responsible for the development of hemolytic uremic syndrome. The recent identification of CD11b as a cellular receptor for leukocidin A/B, a toxin that contributes to the S aureus-mediated killing of neutrophils,86 exemplifies how much our understanding of the neutrophil-pathogen interaction is increasing. Furthermore, recent findings have demonstrated that also neutrophil-derived EVs may contribute to restrict bacterial growth and dissemination, in addition to NETs.87,-89 Accordingly, depending on the nature of the stimulus activating neutrophils, various EVs types have been identified, all with different protein composition and biological properties, as well as exerting antibacterial effects distinct from those of NETs.87,90,91 However, whether neutrophils kill bacteria through NET and EVs release, or instead entrap them only, remains to be definitively solved.5,89,91
Intriguingly, it is now appreciated that neutrophils may actually favor disease progression, depending on the infectious agent.3 For example, it has been shown that neutrophils contribute to the development of Lyme arthritis, a chronic inflammatory conditions occurring several months after Borrelia Burgdorferi infection, by recruiting pathogenic Th1/Th17 clones to the inflamed joint.92 Furthermore, pathogens can evade neutrophil clearance, as recently reported for Neisseria gonorrheae93 or Mycobacterium abscessus,94 which were shown to promote their survival by delaying primary granule-phagosome fusion93 or by inducing a limited pattern of neutrophil activation,94 respectively. Similarly, community-associated methicillin-resistant Staphylococcus aureus has been shown to survive within neutrophil phagosome and inhibit macrophage-mediated efferocytosis of community-associated methicillin-resistant S aureus-infected neutrophils.95 On the same line, the ability of Francisella tularensis to parasitize neutrophils and evade elimination has also been recently reviewed.96
Neutrophils in autoimmunity
It has long been known that poorly controlled neutrophil activation is responsible for much of the tissue/organ damage in a variety of autoimmune diseases. More recently, a number of studies have highlighted the observation that neutrophils are a major source of autoantigens in these diseases.97,98 In this context, “NETting” neutrophils were recently found to release potential autoantigens, including deaminated histones in Felty’s syndrome, proteinase 3, or myeloperoxidase in autoimmune vasculitis, self-DNA, and antimicrobial peptides in SLE or citrullinated histones in rheumatoid arthritis (RA).98,99 There is therefore a strong interest in trying to understand how modified proteins externalized during neutrophil death by apoptosis or “NETosis” can function as autoantigens, leading to loss of tolerance and promoting autoimmune disease development.98 NETs have been shown to act as vehicles for proinflammatory molecules11,100 or tissue factor.101 The latter observation is of particular interest, considering that thrombotic risk is elevated not only in autoimmune vasculitis but also in other chronic diseases in which NETs form, including SLE, RA, colitis, and cancer.89,102 Impairment in NET clearance has also been associated to the pathogenesis of autoimmune diseases such as SLE98 or antiphospholipid syndrome.103 Interestingly, signal inhibitory receptor on leukocytes-1, a surface molecule previously shown to act as a negative regulator of phagocytes,104 can inhibit spontaneous and anti-neutrophil antibody-induced NET formation in SLE, likely by suppressing nicotinamide adenine dinucleotide phosphate oxidase and mitogen activated protein kinase kinase-extracellular signal-regulated kinase activity.105 Thus, recombinant signal inhibitory receptor on leukocytes-1 or other NET inhibitors might be considered for autoimmune disease treatment.98 Finally, human neutrophils have been recently suggested to contribute to the pathogenesis of autoimmune T1D, further confirming what recently observed in mice with spontaneous autoimmune T1D.106 If verified by more comprehensive studies, these data might lead to the definition of new therapeutic strategies for a disease that to date has proved controllable but incurable.106
Neutrophils in cancer
Recent reviews elegantly discuss the multiple (pro- and antitumor) roles of neutrophils in cancer.59,107,108 Current evidence mostly support the idea that neutrophils facilitate, rather than inhibit, cancer progression primarily through their ability to promote tumor angiogenesis, invasion, and metastasis.107,,-110 This concept is also supported by dozens of reports correlating elevated numbers of tumor-infiltrating and/or blood neutrophils, as well as elevated blood neutrophil/lymphocyte ratios, with poor clinical outcome in several cancers.111 The mechanisms whereby neutrophils contribute to cancer metastasis, in particular, have recently gained more attention. For instance, even NETs have been involved in metastasis, by both trapping cancer cells and favoring their dissemination through the microvasculature.112 Histopathological evaluation of biopsies from a small cohort of pediatric patients with Ewing sarcoma has indeed revealed the presence of tumor-associated neutrophils undergoing NETosis in samples from patients with metastasis.113 In this context, we have shown that metastatic tumor-draining lymph nodes from carcinoma patients infiltrated by slanDCs also contain, in some cases, CD66b+neutrophils within an immunosuppressed like microenvironment.114 A very recent observation in a head and neck cancer model suggests that neutrophils, previously exposed to tumor-conditioned medium, induce an invasive, NK-resistant, and highly metastatic tumor cell phenotype (S. Brandau, unpublished data, 2014). Another mechanism proposed to explain protumor activities by human and mouse tumor-associated neutrophils consists in their ability to recruit regulatory T cells (Tregs) to the tumor sites, via CCL17 release.115 Based on all these findings, inducing the conversion of neutrophils from protumor to antitumor cells may represent a new form of immunotherapy for cancer.116 In this context, because neutrophils are the most abundant population of circulating white blood cells expressing FcγR and FcαR able to execute potent cytotoxic functions, the possibility of exploiting neutrophils for antibody-based cancer immunotherapy holds significant promise and deserves further investigation.117
Concluding remarks
It is now beyond doubt that the traditional view of neutrophils as short-lived effector cells with limited functional capacity is incomplete. Neutrophils display many more functions than previously suspected, including the capacity to influence regulatory circuits in the innate and adaptive immune systems. The increasing availability of experimental animal models, including the zebrafish system, which allows prompt genetic and chemical manipulation,118 will provide new approaches to expand our knowledge of neutrophil biology.
As mentioned, an additional way whereby neutrophils may orchestrate, under physiological and pathological conditions, the evolution of inflammation, immune response, hematopoiesis, wound healing, angiogenesis, tissue remodeling, and bone reabsorption, occurs via the production and release of cytokines.13 In this context, as our technologies become more powerful and new molecules are cloned, the number of cytokines and chemokines that neutrophils can potentially produce continues to expand (Table 3), in some cases being regulated in a neutrophil-specific manner.13,57,59 Although the molecular mechanisms underlying the peculiar regulation of cytokine expression in neutrophils remain to be defined, recent studies suggest that they may include neutrophil-specific chromatin organization programs.119 Future challenges for scientists in the field will be to translate all these new insights into efficacious neutrophil-targeted therapies for the treatment of inflammatory conditions without compromising immunity.
Cytokines that human neutrophils can potentially express and/or produce
| Cytokine family . | Specific cytokines . |
|---|---|
| C-X-C chemokines | CXCL1, CXCL2, CXCL3, CXCL4*, CXCL5, CXCL6, CXCL8, CXCL9, CXCL10, CXCL11, CXCL12*, CXCL13* |
| C-C chemokines | CCL2, CCL3, CCL4, CCL17, CCL18, CCL19, CCL20, CCL22 |
| Proinflammatory cytokines | IL-1α, IL-1β, IL-6, IL-7, IL-9(?), IL-16(?), IL-17A, IL-17B, IL-18, MIF |
| Anti-inflammatory cytokines | IL-1ra, IL-4(?), TGFβ1, TGFβ2 |
| Immunoregulatory cytokines | IFNα(?), IFNβ*, IFNγ(?), IL-12, IL-21, IL-23, IL-27, IL-18BP |
| TNF superfamily members | TNFα, TNFSF6/FasL, TNFSF8/CD30L, TNFSF10/TRAIL, TNFSF14/LIGHT*, TNFSF3/Lymphotoxin-β*, TNFSF13/APRIL, TNFSF13B/BAFF/BLyS, TNFSF5/CD40L, TNFSF11/RANKL |
| Colony-stimulating factors | G-CSF, M-CSF(?), GM-CSF(?), IL-3(?), SCF* |
| Angiogenic and fibrogenic factors | VEGFs, BV8 (prokineticin 2), HB-EGF, FGF-2, TGFα, HGF, angiopoietin-1 |
| Other cytokines | NGF*, BDNF*, NT4*, PBEF (visfatin/NAMPT), amphiregulin, midkine, oncostatin M, activin A, endothelin |
| Cytokine family . | Specific cytokines . |
|---|---|
| C-X-C chemokines | CXCL1, CXCL2, CXCL3, CXCL4*, CXCL5, CXCL6, CXCL8, CXCL9, CXCL10, CXCL11, CXCL12*, CXCL13* |
| C-C chemokines | CCL2, CCL3, CCL4, CCL17, CCL18, CCL19, CCL20, CCL22 |
| Proinflammatory cytokines | IL-1α, IL-1β, IL-6, IL-7, IL-9(?), IL-16(?), IL-17A, IL-17B, IL-18, MIF |
| Anti-inflammatory cytokines | IL-1ra, IL-4(?), TGFβ1, TGFβ2 |
| Immunoregulatory cytokines | IFNα(?), IFNβ*, IFNγ(?), IL-12, IL-21, IL-23, IL-27, IL-18BP |
| TNF superfamily members | TNFα, TNFSF6/FasL, TNFSF8/CD30L, TNFSF10/TRAIL, TNFSF14/LIGHT*, TNFSF3/Lymphotoxin-β*, TNFSF13/APRIL, TNFSF13B/BAFF/BLyS, TNFSF5/CD40L, TNFSF11/RANKL |
| Colony-stimulating factors | G-CSF, M-CSF(?), GM-CSF(?), IL-3(?), SCF* |
| Angiogenic and fibrogenic factors | VEGFs, BV8 (prokineticin 2), HB-EGF, FGF-2, TGFα, HGF, angiopoietin-1 |
| Other cytokines | NGF*, BDNF*, NT4*, PBEF (visfatin/NAMPT), amphiregulin, midkine, oncostatin M, activin A, endothelin |
The expression and/or production of most of these cytokines (updated from Mantovani et al3 ) has been validated in human neutrophils by gene expression techniques, immunohistochemistry, enzyme-linked immunosorbent assay, or biological assays. *, studies performed at the mRNA level only; (?), controversial data; APRIL, proliferation-inducing ligand; BAFF/BLyS, B-cell activating factor/B lymphocyte stimulator; BDNF, brain-derived neurotrophic factor; CCL, CC chemokine ligand; CXCL, CXC chemokine ligand; FasL, Fas ligand; FGF, fibroblast growth factor; HB-EGF, heparin binding-like epidermal growth factor; HGF, hepatocyte growth factor; IFN, interferon; IL-1ra, IL-1 receptor antagonist; IL18BP, IL-18 binding protein; LIGHT, homologous to lymphotoxins; M-CSF, macrophage-colony stimulating factor; MIF, macrophage inhibitory factor; NAMPT, nicotinamide phosphoribosyl transferase; NGF, nerve growth factor; NT4, neurotrophin-4; PBEF, pre-B-cell colony-enhancing factor; RANKL, receptor activator of nuclear factor k-B ligand; SCF, stem cell factor; TGF, transforming growth factor; TNFSF, TNF super family; TRAIL, TNF-related apoptosis-inducing ligand; VEGF, vascular endothelial growth factor.
The online version of this article contains a data supplement.
Acknowledgments
We thank C. A. Lowell for critical suggestions and helpful comments.
This work was supported by Associazione Italiana per la Ricerca sul Cancro, grant IG-11782 (M.A.C.) and Ministero dell’Istruzione dell’Universita’ e della Ricerca grant RBFR12I3UB_003 (P.S.).
Authorship
Contribution: P.S. and M.A.C. wrote the review.
Conflict-of-interest disclosure: The authors declare no competing financial interest.
Correspondence: Patrizia Scapini, Department of Pathology and Diagnostics, Section of General Pathology, Strada Le Grazie 8, 37134 Verona, Italy; e-mail: patrizia.scapini@univr.it; or Marco A. Cassatella, Department of Pathology and Diagnostics, Section of General Pathology, Strada Le Grazie 8, 37134 Verona, Italy; e-mail: marco.cassatella@univr.it.