Key Points
Matriptase-2 is required for hepcidin suppression in fetuses and neonates to ensure iron mobilization to avoid iron deficiency and anemia.
In matriptase-2–deficient mice, the constant developmental hyperhepcidinemia is not explained by increased level of hepatic hemojuvelin.
Abstract
Iron is an essential element required for development and survival of all living organisms. In fetuses, maternofetal iron transfer across the placenta is essential for growth and development. In neonates, efficient intestinal iron absorption is required to scavenge as much iron as possible from the low-iron-content milk. During these periods, efficient iron mobilization is ensured by the downregulation of the iron regulatory hormone hepcidin by as-yet uncharacterized molecular mechanisms. Here we demonstrate that the recently described hepcidin repressor—the serine protease matriptase-2 (encoded by Tmprss6)—is responsible for this repression throughout development, with its deficiency leading to increased hepcidin levels triggering iron deficiency and anemia starting in utero. This result might have implications for a better understanding of iron homeostasis during early development in iron-refractory iron deficiency anemia patients, who present with microcytic anemia caused by hyperhepcidinemia, and of questions about the role of matriptase-2 in human neonates.
Introduction
For most living organisms, iron is essential but potentially toxic, making the maintenance of systemic iron homeostasis critical. This homeostasis is orchestrated by the hormone hepcidin, which regulates the amount of the cell membrane iron exporter ferroportin. Hepcidin binds to ferroportin, inducing its degradation and leading to decreased iron availability and hypoferremia.1 Hepcidin regulation is complex and depends on various signals. Among the most important is body iron level (both circulating and intracellular iron) that upregulates hepcidin through the bone morphogenic protein 6 (BMP6) regulatory pathway involving the SMAD signaling cascade. BMP6 binds to types I and II BMP receptors in the presence of hemojuvelin (HJV), a BMP coreceptor. This BMP6/BMP receptor/HJV interaction triggers phosphorylation of SMAD1/5/8 proteins, recruitment of SMAD4, and translocation of the complex into the nucleus to increase hepcidin gene transcription.1 The Hjv-dependent upregulation of hepcidin was recently shown to be interrupted by the type II transmembrane serine protease matriptase-2 (Mt2, encoded by Tmprss6), a repressor of hepcidin expression acting through proteolytic degradation of Hjv.2,3 Null mutations in TMPRSS6 result in the clinical phenotype of iron-refractory iron deficiency anemia hallmarked by inappropriately high hepcidin level4,5 resulting from constitutive hyperactivation of the BMP6/HJV/SMAD pathway.6-8 Thus, by downregulating hepcidin gene expression, Mt2 controls iron availability to avoid systemic iron deficiency. In fetal and neonatal periods, because of the red cell compartment’s rapid growth and expansion, hepcidin gene expression is drastically repressed.9,10 However, the role of Mt2 in this repression has not been addressed and constitutes the aim of this study.
Methods
Animals
Tmprss6−/− mice have been described elsewhere.8,11 Age-matched wild-type (Tmprss6+/+), heterozygous (Tmprss6+/−), and homozygous (Tmprss6−/−) mice were obtained after mating heterozygous males and females (all backcrossed 4 times on a BALB/cOlaHsd). For the study of E17.5 fetuses, Tmprss6+/+ and Tmprss6+/− mice were pooled and named Tmprss6+/?. Control and mutant embryonic day 17.5 (E17.5) fetuses as well as mice at postnatal days 0, 3-4, 7, 14, and 42 were analyzed for iron-related gene expression. When indicated, iron and hematological parameters were evaluated. Animal studies were approved (agreement number CEEA34.BV.157.12) by the “Président du Comité d'Ethique pour l'Expérimentation Animale Paris Descartes.”
RNA extraction, reverse transcription, and quantitative polymerase chain reaction have been previously described.8 Messenger RNA (mRNA) expression was calculated using the ΔΔCt method and normalized to the expression of cyclophilin. Primers used are outlined in supplemental Table 2 on the Blood Web site.
Extraction of membrane and cytosolic fractions were performed as previously described.12 The following antibodies were used: anti-mouse β-actin (ascites fluid reference A5316 from Sigma-Aldrich); anti-mouse TfR1 (TFR16-M from α-diagnostic); anti-mouse ferroportin (MTP11-A from α-diagnostic); and anti-mouse Hjv (AF3634 from R&D Systems). The iron content in fetuses was determined by acid digestion of tissue samples as described by Torrance and Bothwell,13 followed by determination of the iron content by a colorimetric assay on an Olympus AU400 automat. Hematologic parameters were measured on a MS9-5V apparatus (Melet Schloesing Laboratories).
Statistical analysis was performed using nonparametric Mann-Whitney U tests. P values <.05 were considered statistically significant. Detailed information on methods is included in the supplemental Methods.
Results and discussion
Mt2 is required to maintain iron homeostasis during fetal and postnatal development
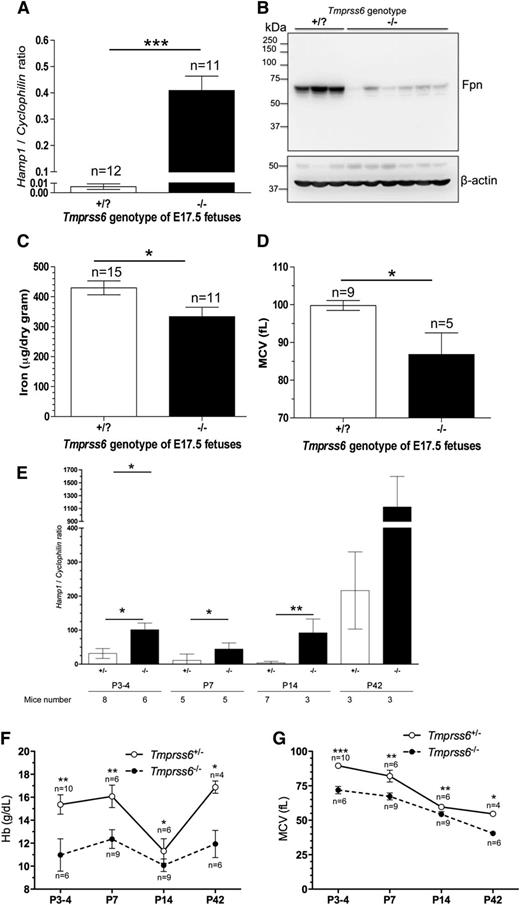
Adult Tmprss6−/− mice were previously shown to excessively express the Hamp1 gene, leading to iron-deficiency anemia.8,11 Tmprss6 transcript levels were found to progressively increase from the fetal stage and through postnatal development (supplemental Figure 1). To address the role of Tmprss6 in iron homeostasis during the fetal period, Tmprss6 heterozygous mice were intercrossed and females were euthanized at E17.5. In E17.5 Tmprss6−/− fetuses, we found a dramatic increase of liver Hamp1 mRNA (up to 60-fold) as compared with controls, in which expression of hepcidin was barely detectable (Figure 1A). To determine the physiological relevance of increased hepcidin gene expression, we analyzed ferroportin expression in the placenta. This transporter ensures iron transfer from the mother to the fetus to cover fetal growth and appropriate hepatic iron reserves.14 We found a strong decrease of membrane ferroportin protein levels in the placenta of the Tmprss6−/− fetuses (Figure 1B), without any change in ferroportin mRNA levels (supplemental Figure 2), supporting a role for hepcidin in placental ferroportin degradation. As a direct consequence of increased hepcidin-induced ferroportin degradation, we measured a reduction in iron content, a significant decrease of the mean corpuscular volume (MCV) (Figure 1C-D), and a trend for hemoglobin (Hb) decrease (supplemental Figure 3) in E17.5 Tmprss6−/− fetuses, hallmarking iron deficiency and microcytic anemia in the mutant fetuses. Red blood cell (RBC) levels, however, were unaffected (not shown). At birth (P0), we similarly found increased hepcidin gene expression and reduced MCV in the Tmprss6−/− pups (supplemental Figure 4). During the critical period of suckling, from P3-4 to P14, we observed, as previously described,9,10 a progressive reduction of liver Hamp1 expression in control mice, with expression being undetectable at P14 (Figure 1E). At weaning, hepcidin gene expression is reactivated, likely in response to decreased erythroid signals and activation of the iron signaling pathway triggered by the iron-rich carbohydrate diet. In contrast, a constantly elevated level of Hamp1 mRNA was detected throughout liver development in Tmprss6−/− neonates compared with controls (Hamp1 expression increased fourfold in Tmprss6−/− adult mice at P42, as reported8 ). As a consequence, Hb and MCV levels, although following the same trend during postnatal development as controls, were significantly lower in Tmprss6−/− mice (Figure 1F-G). Of note, the increased RBC count was similar, independent of the genotype during postnatal development (supplemental Figure 5). Additional hematological parameters are presented in supplemental Table 1. Altogether, these results demonstrate that Mt2 is required for hepcidin repression during fetal and postnatal development, and its deficiency leads to a microcytic anemia in utero and in neonates, which persists to adult stages.
Results of hyperhepcidinemia in the livers of E17.5 Tmprss6−/− fetuses and during postnatal development on iron homeostasis and hematological parameters. The phenotype analyzed in E17.5 fetuses include liver Hamp1 mRNA levels relative to Cyclophilin expression assessed by quantitative polymerase chain reaction (A); placenta ferroportin (FPN), membrane protein expression assessed by western blot analysis with β-actin as a loading control (B) (quantification of the membrane was performed using ImageJ and is presented in supplemental Figure 7); total nonheme body iron (C); and MCV (D). The phenotype analyzed during postnatal development included liver Hamp1 mRNA (E), Hb (F), and MCV (G). Data are presented as mean ± standard deviation. *P < .05; **P < .005; ***P < .0005
Results of hyperhepcidinemia in the livers of E17.5 Tmprss6−/− fetuses and during postnatal development on iron homeostasis and hematological parameters. The phenotype analyzed in E17.5 fetuses include liver Hamp1 mRNA levels relative to Cyclophilin expression assessed by quantitative polymerase chain reaction (A); placenta ferroportin (FPN), membrane protein expression assessed by western blot analysis with β-actin as a loading control (B) (quantification of the membrane was performed using ImageJ and is presented in supplemental Figure 7); total nonheme body iron (C); and MCV (D). The phenotype analyzed during postnatal development included liver Hamp1 mRNA (E), Hb (F), and MCV (G). Data are presented as mean ± standard deviation. *P < .05; **P < .005; ***P < .0005
Decrease of membrane Hjv in the liver of Tmprss6−/− mice is not due to iron deficiency or anemia
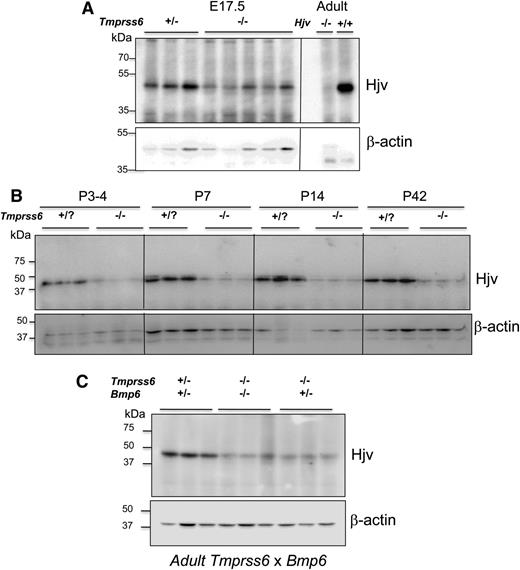
From the in vitro demonstration of Hjv degradation by Mt2,3 hyperhepcidinemia in Tmprss6−/− mice was anticipated to result from increased membrane Hjv and activated BMP6/SMAD pathway. However, Krijt et al reported that Hjv content was decreased in Tmprss6−/− liver mice.15 Here, we confirmed and further extended this result by showing a drastic reduction of membrane Hjv in the liver of E17.5 Tmprss6−/− fetuses (Figure 2A) and during the postnatal development (Figure 2B) as compared with controls, without alteration of Hjv mRNA level (supplemental Figure 6). We hypothesized that this Hjv decrease could result from a counterregulation of the Tmprss6−/− mice to combat the anemia. To address this question, we looked at Hjv levels in the liver of mice deficient for Mt2 but rescued for their anemia in the double knockouts Tmprss6/Bmp6.8 As shown in Figure 2C, the amount of liver membrane Hjv was similarly reduced in anemic Tmprss6−/−Bmp6+/− mice and in the rescued double-mutant Tmprss6−/−Bmp6−/− mice, suggesting that the lack of Mt2 per se is responsible for Hjv reduction, and is independent of iron deficiency and anemia.
Reduction of hepatic membrane HJV protein in Tmprss6−/− E17.5 fetuses and neonates. Analysis of liver membrane Hjv protein in Tmprss6−/− E17.5 fetuses (A) and during postnatal development (B) or in adult Tmprss6 × Bmp6 mice (C) assessed by immunoblot analysis. A representative blot is presented. A sample from an adult Hjv−/− mouse was used to control the specificity of the Hjv-related band. Antibody recognizing β-actin was used as a loading control. Quantification was performed using ImageJ and is presented in supplemental Figure 7.
Reduction of hepatic membrane HJV protein in Tmprss6−/− E17.5 fetuses and neonates. Analysis of liver membrane Hjv protein in Tmprss6−/− E17.5 fetuses (A) and during postnatal development (B) or in adult Tmprss6 × Bmp6 mice (C) assessed by immunoblot analysis. A representative blot is presented. A sample from an adult Hjv−/− mouse was used to control the specificity of the Hjv-related band. Antibody recognizing β-actin was used as a loading control. Quantification was performed using ImageJ and is presented in supplemental Figure 7.
In conclusion, our study indicates that Mt2 is required to repress hepcidin gene expression during development to limit iron deficiency and anemia. This finding should be taken into consideration because iron deficiency is considered the most common nutritional deficiency in humans. Our results might have implications to better understand iron homeostasis during early development in iron-refractory iron deficiency anemia patients. Our work also confirms that there is no correlation between the amount of Hjv present in the liver membrane and hepcidin gene expression, although this result will benefit from validation using other anti-Hjv antibodies. Interestingly, repression of hepcidin by increased erythroid activity (phlebotomy or erythropoietin injection) was recently reported to be due to a circulating factor named erythroferrone, which is produced by erythroblasts.16 We have previously demonstrated that Tmprss6−/− mice have higher plasma erythropoietin levels, but that the signaling leading to Hamp1 repression was not functional.17 It is therefore tempting to speculate that erythroferrone requires Mt2 to efficiently repress liver hepcidin expression in response to elevated erythropoiesis (as seen during development when RBC content gradually increased by fourfold), a hypothesis that deserves further investigation.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Nancy C. Andrews (Department of Pharmacology and Cancer Biology, Duke University, Durham, NC), Zoubida Karim (Centre de Recherche Biomédicale Bichat Beaujon CRB3, Paris, France), and Drs Marie-Paule Roth and Hélène Coppin (UMR1043, Toulouse, France) for kindly providing the Hjv−/− samples and the Bmp6−/− mice, respectively. The authors also thank the staff of their animal facility.
This study was supported by grants from the French National Research Agency Blanc (2010 1130 01) and from the Laboratory of Excellence GR-Ex (ANR-11-LABX-0051), which is funded by the program “Investissements d’avenir” of the French National Research Agency (ANR-11-IDEX-0005-02).
Authorship
Contribution: A.W., A.L., J.-C.D., and G.N. performed experiments; G.N. and S.V. conceived, analyzed, and interpreted the experiments; C.L.-O. and A.J.R. provided the Tmprss6 knockout model; and G.N. and S.V. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Gaël Nicolas, Institut Cochin, Département Endocrinologie Métabolisme et Diabète, INSERM U1016, CNRS UMR8104, 24 rue du Faubourg Saint Jacques, 75014 Paris, France; e-mail: gael.nicolas@inserm.fr; and Sophie Vaulont, Institut Cochin, Département Endocrinologie Métabolisme et Diabète, INSERM U1016, CNRS UMR8104, 24 rue du Faubourg Saint Jacques, 75014 Paris, France; e-mail:, sophie.vaulont@inserm.fr.
References
Author notes
S.V. and G.N. contributed equally to this study.