Abstract
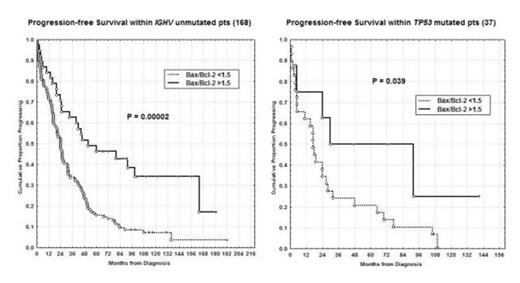
Impaired programmed cell death is an important factor both in the pathogenesis of CLL (Berndt et al, Nat Genet 2013) and in the development of resistance to chemoimmunotherapy (Fegan et al, Adv Exp Med Biol 2013). It has become increasingly clear that in CLL the balance between the pro- (Bax) and anti-apoptotic members (Bcl-2) of the Bcl-2 family determines the chemotherapy sensitivity and ultimately progression free (PFS) and overall survival (OS). Moreover, the today availability in clinical use of novel potent oral pro-apoptotic BH3 peptidomimetics such as ABT 199 (Seymour et al, ASH 2013) emphasized the importance of Bcl-2 family-targeted therapy, prompting us to analyze the real impact of Bax/Bcl-2 ratio on CLL prognosis. The primary aims of our research were: 1) to correlate Bax/Bcl-2 ratio with other clinical and biological prognostic factors; 2) to determine PFS and OS upon Bax/Bcl-2 ratio; 3) to confirm Bax/Bcl-2 as an independent prognostic factor. Therefore we investigated 502 pts, median age 65 years (range 33-89), 279 males and 223 females. With regard to modified Rai stages at diagnosis, 170 patients had a low stage, 318 an intermediate stage and 14 a high stage. Bax/bcl-2 ratio was calculated by flow cytometry, dividing mean fluorescence intensity (MFI) of bax by MFI of bcl-2 on CD19+CD5+ CLL cells. The threshold was set at the median value >1.5 (range 0.27-6.10). Two hundred sixty- six patients were Bax/Bcl-2 ratio positive (266/502; 53%). Higher Bax/Bcl-2 ratio was significantly associated with low Rai stage, lymphocyte doubling time >12 months, beta-2 microglobulin <2.2 mg/dl and soluble CD23<70 U/ml (P<0.0001). Moreover, higher Bax/Bcl-2 was greatly represented within the low risk (normal or del13q) cytogenetics (221/341; P<0.0001). Noteworthy, significant correlations were found between lower Bax/Bcl-2 ratio and IGHV unmutated status (130/168; P<0.0001) or NOTCH1 (49/58; P<0.0001) or TP53 mutations (29/37; P=0.00007). With regard to clinical outcome, significant shorter PFS and OS were observed in patients with lower Bax/Bcl-2 ratio (10% vs 52% at 16 years; P<0.0001 and 46% vs 79% at 16 years; P<0.0001, respectively). To further explore the prognostic impact of Bax/Bcl-2 ratio, we investigated its expression within IGHV unmutated (168 pts) and TP53 mutated subgroups (37 pts), notoriously at worst prognosis. As a matter of fact, higher Bax/Bcl-2 ratio identified patients with a significant longer PFS (43% vs 10% and 50% vs 10% at 7 years; P=0.00002 and P=0.039, respectively, Figure), so suggesting its very high prognostic impact. In multivariate analysis of PFS (489 patients), Bax/Bcl-2 ratio (P<0.0001) together with modified Rai stages (P<0.0001), cytogenetics (P=0.0001), IGHV status (P<0.0001) and TP53 (P=0.001) was confirmed to be an independent prognostic factor. Therefore, the apoptotic index Bax/Bcl-2, performed by flow cytometry, is a powerful prognostic marker being able to identify patients at different prognosis also within IGHV unmutated and TP53 mutated subsets which are at very high risk. The modern strategies to downregulate Bcl-2 and shift the balance toward cellular demise, such as the BH3 mimetic ABT 199, could be carefully and precisely monitored by using this simple but powerful flow cytometric approach.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal