Abstract
Background: Low-risk myelodysplastic syndrome (LR-MDS) is a heterogeneous group of diseases characterized by dysplastic ineffective hematopoeisis and risk for acute myelogenous leukemia (AML). Despite improved risk classification, LR-MDS subgroups exhibit outcome heterogeneity. Non-hemopoeitic comorbidities highlight interaction of organ dysfunction and adverse outcomes. Previous studies have identified association between smoking and development of MDS (Du Y. Leuk Res. 2010). Among others, smoking induces DNA double strand breaks (Huang et al, 2012) and gene methylation modification leading to impaired environmental chemicals detoxification. In this study, we analyze the clinical impact of smoking and intensity of exposure on LR-MDS outcome.
Methods: With prior IRB approval, 90 LR-MDS patients from the Michael E. DeBakey VA Medical Center cancer registry were analyzed between 2000-2012. Smoked pack-years (PY) was recorded according to accepted definition. PY estimate derived from Framingham heart study (Mannan H et al., Heart International. 2010) was used to evaluate smoking dose-dependent correlation with survival in: (1) non-smoker [NS], (2) <20, (3) >20-39, and (4) >40 PY. Univariate and multi-variable analysis evaluated the impact of potential confounding variables such as degree of cytopenia at disease initiation, blast count, karyotype, and R-IPSS score.
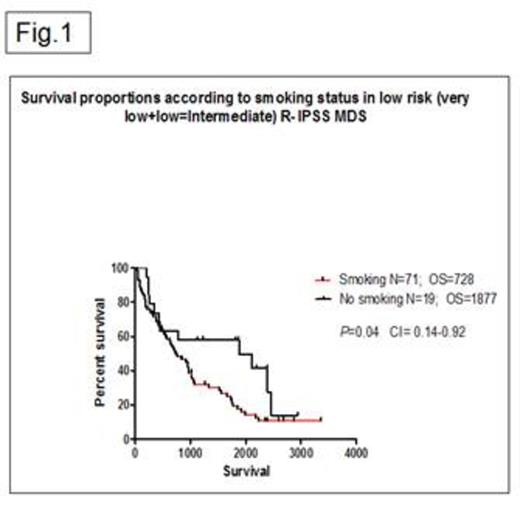
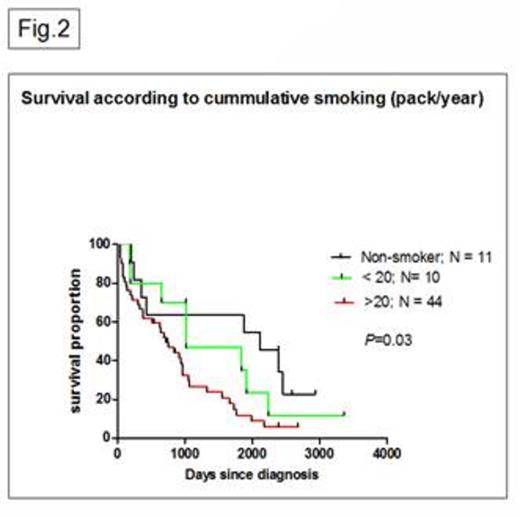
Results: 69 (76%) and 22 (24%) pts were smokers and NS. Median age was 71 years (y) (range, 55-84) and 73 y (60-87), for smokers and NS, P=0.38. 22 (24%), 35 (38%) and 34 (37%) of pt were very low, low, and intermediate risk R-IPSS. Median hemoglobin, ANC, and platelet levels among smokers and NS were 9.4 g/dL vs 8.8 g/dL (P=0.18), 2.7 K/uL vs 3.2 K/uL (P=0.13) and 118 K/uL vs 158 K/uL (P=0.11). Median absolute R-IPSS score for smokers and NS were 0.5 (range, 0-1.5) and 0.25 (range, 0-2), P=0.40. OS in smokers vs NS was 728 vs 1877 days (d), P=0.04, 95% CI= 1.015 to 2.923 (Fig. 1). 65/71 (92%) pt contributed to analysis of cumulative effect of smoking on OS. Given the lack of significant survival difference among pt with >20-39 and >40 PY, 3 distinct subgroups were identified showing a median OS of 2117, 1020 and 717 d, for NS, <20 and >20 PY, respectively, P=0.01 (Fig. 2). Univariate and multivariate analysis revealed no impact of blast count, depth of cytopenias, karyotype, and R-IPSS on observed outcomes.
Conclusions: Our study suggests a mechanistic link between smoking and adverse outcome in LR-MDS. Higher cumulative smoking exposure is potentially associated with worse OS. Larger studies involving LR-MDS pt with smoking history are necessary to confirm this association. Further research is needed to clarify underpinning mechanisms resulting in unfavorable smoking-induced LR-MDS phenotype. This could facilitate implementation of MDS directed therapy in subgroups with more aggressive outcome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal