Abstract
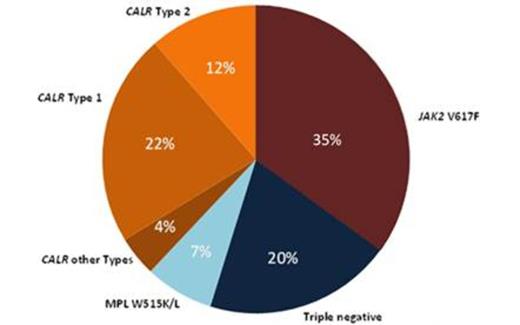
Bleeding and thrombotic events are major clinical complications of ET, together with progression to myelofibrosis and leukemic transformation (AML). The JAK2 V617F mutation, the thrombopoietin receptor mutation MPL W515K/L and the most recently discovered calreticulin (CALR) mutations are mutually exclusive in ET, account for up to 80-90 % of ET cases and support a novel molecular categorization of ET. In a retrospective study, we have examined the clinical phenotype and outcome of a Belgian cohort of 165 ET patients in relation to their mutational status. 38% of the patients were CALR mutated, 22% and 12% of whom carried Type 1 (p.L367fs*46) and Type 2 (p.K385fs*47) indels respectively. 35% were JAK2 V617F positive, 7% were MPL W515K/L positive, one patient was positive for both CALR and JAK2 V617F mutations, and 20% were triple negative (Fig. 1). We compared the hematological and clinical features between CALR mutant patients and JAK2 V617F positive patients. This revealed that CALR mutant ET is associated with younger age than JAK2 V617F positive ET (median age 56 y (range 23-84) versus 65 y (range 36-94), p<0.001), male gender (58% versus 39%, p=0.03), higher platelet count (988 ± 367*109/L versus 870 ± 291*109/L, p=0.04 (mean ± SD)), lower leukocyte count (9.1 ± 3.2*109/L versus 11.6 ± 5.8*109/L, p<0.001), lower erythrocyte count (4.36 ± 0.9*1012/L versus 4.98 ± 0.65*1012/L, p<0.001), hemoglobin (13.2 ± 1.8 g/dL versus 14.3 ±1.6 g/dL, p=0.001) and hematocrit (40 ± 6.2 % versus 44 ± 4.6 %, p<0.001). Analysis of the CALR mutant group according to the indel type showed that CALR Type 1 deletion is strongly associated with male gender (62%). Contrary to previously published findings, we did not find significant differences between CALR type I and II mutations with regard to age and platelet count.CALR mutant patients had a better overall survival than JAK2 V617F positive patients (mean survival 28 y versus 16 y, p=0.01). However, the better overall survival for CALR mutant ET was restricted to patients less than 60 years old (mean survival 29.2 y versus 18.5 y, p=0.02) while in the age group above 60 years, the overall survival was not significantly different (mean survival 18.3 y versus 13 y, p=0.32) (Fig. 2). In our cohort, no difference in myelofibrosis-free survival or leukemia-free survival was found between the molecular subtypes, although the risk of developing myelofibrosis was unexpectedly higher in the CALR mutant group (18% versus 4%, p=0.01). In contrast to other studies, we found no difference in the frequency of arteriovenous complications. In conclusion, this study on a Belgian cohort supports the notion that CALR mutant ET is phenotypically distinct from JAK2 V617F positive ET, with regard to the clinical and hematological presentation as well as the overall survival. In this cohort, the better overall survival was most marked in ET patients less than 60 y of age. Our study adds to the growing body of evidence that CALR mutant ET is a disease entity distinct from JAK2 V617F positive ET.
Distribution of 165 ET patients according to their mutational status.
Overall survival of CALR mutant and JAK2 V617F positive groups stratified according to age: older than 60 y versus younger than or equal to 60 y.
Overall survival of CALR mutant and JAK2 V617F positive groups stratified according to age: older than 60 y versus younger than or equal to 60 y.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal