Abstract
Background: In Hodgkin lymphoma (HL) the malignant Hodgkin Reed-Sternberg (HRS) cells comprise only a small fraction of the total cellular tumor population. These HRS cells orchestrate an inflammatory microenvironment of reactive cells that propagate a permissive milieu for HL growth, contributing to an ineffective local anti-tumor immune response. The peritumoral CD4 and CD8 T cells in HL patients show high expression of the receptor programmed death-1 (PD-1), involved in the functional impairment and “exhaustion” of T cells. Growing data suggests that this HL-mediated immune suppression may have effects that extend beyond the tumor microenvironment. High systemic levels of inflammatory cytokines and chemokines in HL patients has been reported. We characterized the systemic immune profile of HL patients with both newly diagnosed (ND) and relapsed (R) disease.
Methods: Informed consent for correlative blood testing was obtained from patients with ND (n=8) or R (n=5) HL treated at the NYU Perlmutter Cancer Center or NY Presbyterian/Weil Cornell since January of 2013. Blood samples were drawn pre-treatment, and at sequential timepoints during and after therapy. Peripheral blood mononuclear cells (PBMC) were isolated using Ficoll separation method and cells were frozen for subsequent analysis. The frozen PBMC were then stained with fluorescent-conjugated antibodies against T cell surface molecules in 10-color FACS analysis. The analyses were performed after gating live cells for CD4, CD8 and memory and effector T cell markers. Patient samples were compared to normal controls matched for age and sex (n=18).
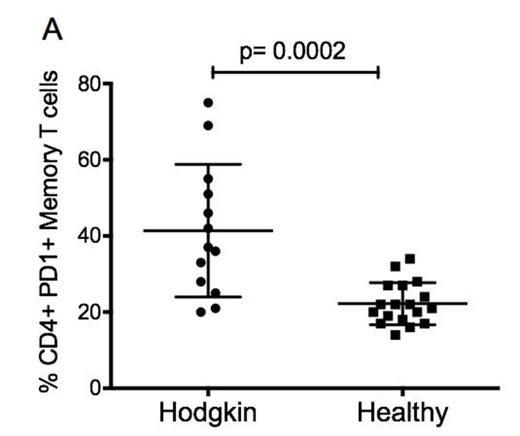
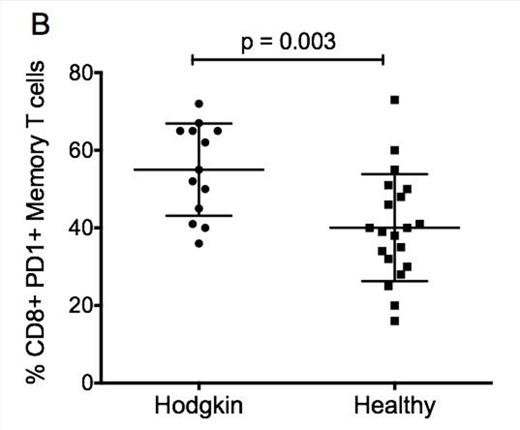
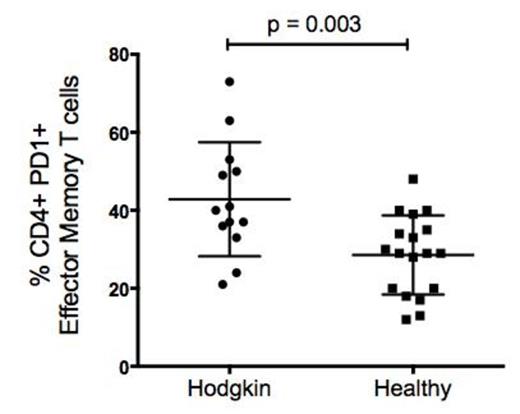
Results: The median HL patient age was 32 (22-72), and 8 subjects were male. All ND HL patients were treated with ABVD (range 4-6 cycles) +/- consolidative radiation; R patients had median of 3 prior therapies. One patient out of 5 had prior autologous stem cell transplant (SCT), and 1 had prior allogeneic SCT, but was not on immunosuppression. Eight patients (6ND, 2R) responded to therapy (8 CR); 5 patients (1ND, 4R) progressed on therapy or had stable disease. HL patients displayed a high frequency of the exhaustion marker PD-1 on CD4 central memory T cells (CD4+CD45RO+CD27+) compared to normal matched controls (NC): mean 41, standard error (SE) 4.8 for HL patients vs. mean 22.2, SE 1.3 for NC (p = 0.0002) (Figure 1A). PD-1 expression was similarly elevated on CD8 central memory T cells (CD8+CD45RO+CD27+) of HL patients: mean 55, SE 3.3 vs. NC: mean 40, SE 3.3 (p = 0.003) (Figure 1B). HL patients also displayed an increased frequency of PD-1 expression on CD27 negative CD4 effector T cells: mean 43, SE 4, vs. NC: mean 28.5, SE 2.4 (p = 0.003) (Figure 2). In 4 of the HL patients who responded to therapy, PD-1 expression on central memory CD4+ cells declined after therapy: mean 30.1 vs. mean increase of +2.67 in 3 patients who progressed on therapy (p< 0.009). A higher number of subjects in prospective analysis is underway, to confirm whether a response to therapy may be correlated with a reversal of the suppressed phenotype of T cells in these patients.
Conclusion: HL patients have evidence of chronic activation/exhaustion in their central memory and effector T cells, suggesting that ineffective immune clearance of the HRS cells may be a systemic rather than local phenomenon. In patients with progressive disease for whom this phenotype persists it is worthy of investigation whether this immune dysfunction is a cause or consequence of resistance to therapy. This may be rationale for immune targeted therapy in patients with relapsed or resistant disease.
Evidence for increased levels of T cell exhaustion in central memory T cells of HL patients. PBMC were stained with specific fluorescent conjugated antibodies against T cell markers (CD3, CD4, CD8) together with differentiation markers (CD45RO, CD27) and PD1 and analyzed using FACS (LSR-II). The proportion of PD1+ T cells were determined in: A) CD4+CD45RO+CD27+ and B) CD8+CD45RO+CD27+ T cells.
Evidence for increased levels of T cell exhaustion in central memory T cells of HL patients. PBMC were stained with specific fluorescent conjugated antibodies against T cell markers (CD3, CD4, CD8) together with differentiation markers (CD45RO, CD27) and PD1 and analyzed using FACS (LSR-II). The proportion of PD1+ T cells were determined in: A) CD4+CD45RO+CD27+ and B) CD8+CD45RO+CD27+ T cells.
Evidence for increased levels of T cell exhaustion in effector memory CD 4+ T cells of HL patients. PBMC were stained with specific fluorescent conjugated antibodies against T cell markers (CD3, CD4) together with differentiation markers (CD45RO, CD27) and PD1 and analyzed using FACS (LSR-II). The proportion of PD1+ T cells was determined in CD4+RO+CD27- T cells
Evidence for increased levels of T cell exhaustion in effector memory CD 4+ T cells of HL patients. PBMC were stained with specific fluorescent conjugated antibodies against T cell markers (CD3, CD4) together with differentiation markers (CD45RO, CD27) and PD1 and analyzed using FACS (LSR-II). The proportion of PD1+ T cells was determined in CD4+RO+CD27- T cells
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal