Abstract
Introduction: Acute myeloid leukemia (AML) is the most common acute leukemia in adults with a median age at diagnosis of 66 years. Over half of the patients are diagnosed at age 65 or older and have shown no improvement in outcomes compared to younger patients in last few decades. The goal of the study was to examine the patient characteristics associated with receiving treatment and the survival outcomes in an older population in routine clinical practice.
Methods: This retrospective cohort analysis utilized data from the linked Surveillance, Epidemiology, and End Results (SEER)-Medicare database. The database is a nationally representative collection of Medicare patients in 18 population-based SEER cancer registries from diverse geographic areas representative of about 26% of the United States population. The analysis included 8336 first primary AML patients diagnosed between January 1, 2000 to December 31, 2009, >66 years, and continuously enrolled in Medicare Part A and B with no HMO coverage in the year prior to diagnosis. Chi-square test for categorical variables and ANOVA or t-test for continuous variables was used to assess differences in patient and disease related characteristics by treatment status. Kaplan-Meier curves and Cox proportional hazards regression assessed survival by treatment status adjusting for age, sex, race, prior myelodysplastic syndrome (MDS), poor performance indicators (PPI), comorbidity, income, education, marital status, year of diagnosis and geographic region. Logistic regression modelling assessed patient characteristics predictive of not receiving treatment.
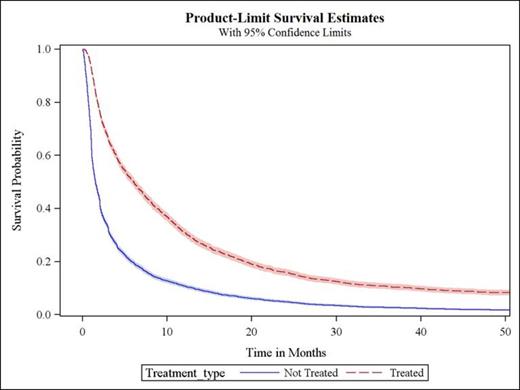
Results: There were 3327 (40%) patients who received treatment with chemotherapy within 3 months of diagnosis and 5009 (60%) patients who did not receive treatment. Treatment rates increased over the study time-period from 35% in the year 2000 to 50% in 2009 (p<.0001). Treated patients were younger (75 vs. 81 years), more likely male (55% vs. 50%), married (61% vs. 47%), lower incidence of antecedent hematologic malignancy (15% vs. 19% prior MDS), less likely to have poor performance indicators (7% vs. 17%) and had lower comorbidity score (p<.0001) than untreated patients. In the treated cohort, 57%, 25%, 10% and 8% had NCI comorbidity score of 0, 1, 2, and ≥3 respectively. In the untreated cohort, 47%, 25%, 14% and 14% had NCI comorbidity score of 0, 1, 2, and ≥3 respectively. The most common comorbidities were hypertension (51%), hyperlipidemia (33%), coronary artery disease (25%), diabetes (21%), and atrial fibrillation (19%). In the logistic regression analysis, increasing age, increasing comorbidity score, black race, prior MDS and PPI were shown to significantly decrease the likelihood of receiving treatment. The median unadjusted overall survival was 2.5 months for the overall population and was longer for treated patients (6.1 months) compared to untreated patients (1.5 months; log rank p <.0001; Figure 1). In multivariate survival analysis, treated patients exhibited a 43% lower risk of death compared to untreated patients (HR=0.57; 95% CI=0.54-0.60). Increasing age, increasing comorbidity score and PPI were significantly associated with higher mortality risks.
Conclusions: Although therapy use has increased over time, this large observational study showed that about 60% of elderly AML patients remain untreated following diagnosis. In the multivariate survival analysis, use of anti-leukemic therapy was associated with significant survival benefit in this cohort of patients. These results suggest an opportunity to improve treatment strategies and delivery to optimize patient outcomes in elderly AML patients.
Unadjusted Overall Survival
Satram-Hoang:Genentech, Inc.: Consultancy. Reyes:Genentech, Inc.: Employment. Hurst:Genentech, Inc.: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal