Abstract
Activating mutations of the BRAF kinase (BRAF V600E) are found in virtually all cases of classical hairy-cell leukemia (HCL), suggesting disease-specific oncogene dependence. Case reports and early trial data demonstrate impressive activity of BRAF inhibitors, but optimal dosing and treatment duration remain unclear.
Methods: We report on 21 patients with hairy cell leukemia across Europe (Heidelberg, Innsbruck, Nice, Munich, Cambridge, Erfurt, Freiburg, Luzern, Cologne, Leicester, London) treated with vemurafenib, a specific BRAF inhibitor outside of trials from 2011-2014. Centers provided clinical data and pathology specimen where available.
Results: Presence of the BRAFV600E mutation was demonstrated in all patients. Median age of all patients included in this study was 64 (range 45-89) years. Patients received a median of 3 (range 0 to 12) prior treatment lines. Two patients were treated upfront (age, comorbidity). Median time between initial diagnosis and experimental treatment with vemurafenib was 8 (range 0-31) years. Vemurafenib was started at a dose of 240 mg bid in 18 patients and was continued at this dose in 14 patients. In four patients doses were escalated to 720 mg (n=1) and 960 mg (n=3), respectively. Three patients received 480 mg (n=2) bid or 960 mg (n=1) bid upfront. Median therapy duration was 90 (range 55-167) days, and 2 patients are still on therapy (day 85 and 275) at last follow up.
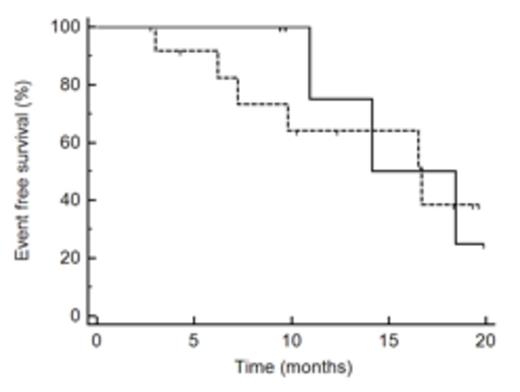
All patient's blood counts improved meeting response criteria (Hb > 12g/dl, platelets 100.000/ µl, neutrophils >1000µl), except for a 89-year-old patient who did not improve with his hemoglobin due to renal anemia. Median time to neutrophil recovery (>1000/ µl) was 39 (range 9-126) days, to platelet recovery (>100.000 µl) 28 (range: 10-105) days and time to improvement of anemia (Hb > 12 g/dl) 67 (range: 10-105) days, respectively. Seven patients achieved a CR and 13 a PR. Patients who received more than 240 mg bid (n=8) did not have significant more CRs than patients who received 240 mg (n=14) (Fishers test p=0.16). CR did not translate into better EFS (HR 1.2, p=0.7, Figure 1 ). Immune histology staining was performed to assess p-ERK signaling.
Median observation time was 12 months (range: 3-31 months) and median event free survival (retreatment or death) was 17 months for all patients (Figure 1). Survival at 12 months was 87%. Three of 21 patients died; one patient due to HCL disease progression after termination of vemurafenib, one patient developed an AML M6 and one patient died at the age of 89 years due to pneumonia off treatment in remission. Seven patients (28%) including the 2 patients treated upfront were retreated at relapse after a median of 10 months (range: 4-16 months) after stopping vemurafenib. Six patients were reexposed to vemurafenib and one received cladribine. All patients responded again to vemurafenib and two patients continue to receive ongoing treatment at 240mg bid and 480mg bid respectively, 18 months and 8.5 months from restarting therapy.
Conclusion: Targeting a BRAF V600E can provide disease control in HCL. CR was achieved in 30% of patients and can be achieved with 240 mg bid. Relatively short EFS suggests that treatment duration and dosing regimen should be optimized and combination treatments involving BRAF inhibitors should be explored in refractory HCL patients. Moreover, dosing schedules and treatment duration may need to be individualized in patients with HCL carefully taking into account individual pharmacodynamics and response.
EFS (re-treatment or death) of HCL patients after vemurafenib treatment. Patients with CR (solid line) and patients with PR (dashed line) have similar EFS.
EFS (re-treatment or death) of HCL patients after vemurafenib treatment. Patients with CR (solid line) and patients with PR (dashed line) have similar EFS.
Herold:Roche Pharma AG/Germany: Honoraria, Research Funding. Dearden:Roche, GSK, Gilead, Janssen, Napp: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal