Abstract
Background:
Several validated prognostic models exist for patients (pts) with MDS, including the International Prognostic Scoring System (IPSS), the Revised IPSS (IPSS-R), and the MD Anderson Prognostic Scoring System (MDAPSS). All were developed in pts with newly diagnosed MDS, and their prognostic value in subsequent stages of disease, such as at the time of failure of hypomethylating agents (HMAs, azacitidine (AZA) and decitabine (DAC), has not been established. Despite this, the IPSS is often used to determine clinical trial eligibility for pts who fail HMAs and is being considered for drug labeling for this indication.
Methods
Clinical data were combined from the MDS Clinical Research Consortium institutions (Moffitt Cancer Center n=259, Cleveland Clinic n=221, MD Anderson Cancer Center n=192, Cornell University n=100, Dana-Farber Cancer Institute n=45, and Johns Hopkins n=29). The IPSS, IPSS-R, and MDAPSS were calculated at the time of diagnosis and HMA failure. HMA failure was defined as no response to AZA or DAC following ≥ 4 cycles, loss of response, or progression to acute myeloid leukemia (AML). Responses were defined per International Working Group criteria (IWG 2006). Overall survival was calculated from the time of HMA failure to time of death or last follow up (OSHF). Survival curves were compared using stratified log-rank tests. Akaike information criterion (AIC) was used to compare fits from Cox proportional hazards models.
Results
A total of 488 pts who failed HMAs and had clinical data available at the time of failure were included in the final analyses. Overall, 406 (83%) were treated with AZA and 82 (17%) with DAC. At diagnosis: median age was 70 years (26-91), median absolute neutrophil count 1.06 k/mL (0.06-36.41), hemoglobin 9.3 g/dL (3.4-38.6), platelets 75 X 103/mL (2-969), and bone marrow blasts 7% (0-28). Prognostic scoring systems at diagnosis included, IPSS: 6 (2%) low, 46 (14%) intermediate-1, 206 (60%) intermediate-2, 83 (24%) high; IPSS-R: 3 (1%) very low, 12 (4%) low, 49 (16%) intermediate, 114 (37%) high, 129 (42%) very high; and MDAPSS: 11 (4%) low, 36 (13%) intermediate-1, 89 (31%) intermediate-2, 149 (52%) high. With median follow up from diagnosis of 18.2 months (mo) (0.7-224.6), median time from diagnosis to HMA start was 1.3 mo (0-162.4). Median number of HMA cycles received was (6, range 4-51): AZA (6, range 4-51), and DAC (4, range 4-21). Median OS from time of diagnosis was 19.5 mo (95% CI, 18.3-22.0).
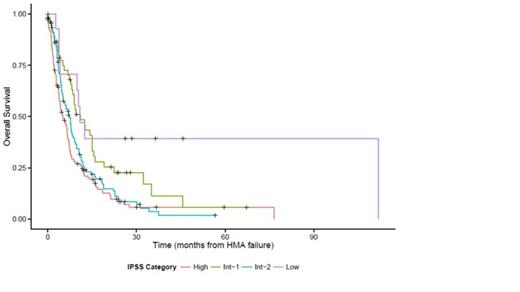
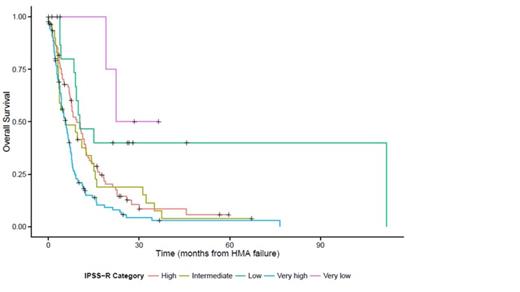
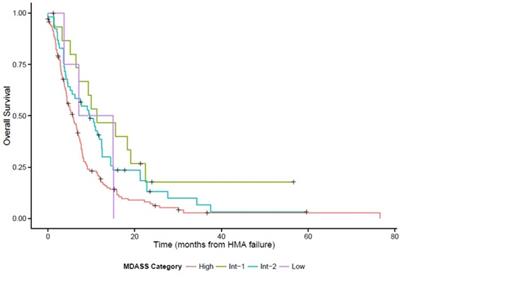
At the time of HMA failure, the median OSHF was 7.1 mo (95% CI, 6.2-7.9). Median OSHF by IPSS (n=311, low 10.9, intermediate-1 11.0, intermediate-2 7.1, high 5.1, p=.005), IPSS-R (n=285, very low 22.4, low 10.3, intermediate 5.6, high 9.4, very high 5.7, p<.0001) and MDAPSS (n=215, low 11.0, intermediate-1 11.3, intermediate-2 9.7, high 5.2, p=.01), Figure 1. Prognostic scoring system comparisons using the subset with all three scores gave AIC values of 1401 (IPSS), 1391 (IPSS-R) and 1393 (MDAPSS), with lower scores indicating a better fit.
Conclusion
When applying three of the most widely used prognostic scoring systems in MDS to pts at the time of HMA failure, the IPSS-R performed the best, followed by the MDAPSS and the IPSS. No system was ideal, though, and should be used with caution for clinical trial eligibility or drug labeling in MDS pts failing HMAs.
Overall survival by scoring systems: (A) IPSS, (B) IPSS-R, (C) MDAPSS
Overall survival by scoring systems: (A) IPSS, (B) IPSS-R, (C) MDAPSS
Roboz:Novartis: Consultancy; Agios: Consultancy; Celgene: Consultancy; Glaxo SmithKline: Consultancy; Astra Zeneca: Consultancy; Sunesis: Consultancy; Teva Oncology: Consultancy; Astex: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal