Abstract
INTRODUCTION AND AIMS: Abnormalities of chromosome 1 (chr 1) are frequently found in hematopoietic stem cell disorders, but their impact and prognosis in Myelodysplastic Syndrome (MDS) remains unclear. For this reason, we retrospectively analyzed a large series of patients.
MATERIALS AND METHODS: A series of 90 patients with MDS and abnormalities of chr 1 were retrospectively evaluated, coming from the Spanish Registry of MDS (68), Marqués de Valdecilla Universitary Hospital (16) and Azienda Careggi Universitary Hospital (Florence) (6). We compared this group to a control group of 992 patients with MDS and an abnormal karyotype, but without abnormalities of chr 1, included in the Spanish Registry of MDS.
RESULTS: Abnormalities of chr 1 occurred in 8.3% of patients with MDS. Fifty seven percent belonged to the high/very high IPSS-R (Revised International Prognostic Scoring System) risk group. The median number of chromosomal abnormalities in the group with and without chr 1 involvement was 3.5 (1-15) and 1 (1-18), respectively (p<0.0001). A complex karyotype was found in 60% and in 16% of patients with and without abnormalities of chr 1, respectively (p<0.0001). The most frequent type of cytogenetic abnormality was translocation (30%). Long arm involvement was seen in 37.8% of patients whereas both arms were only affected in 14.4%. Forty three and thirty one percent of patients with abnormalities of chr 1 had also chr 5 and chr 7 affected, respectively. A low platelet count (<100 x 109/l) was more frequently found in patients with abnormalities of chr 1 (50% vs 32%; p=0.002).
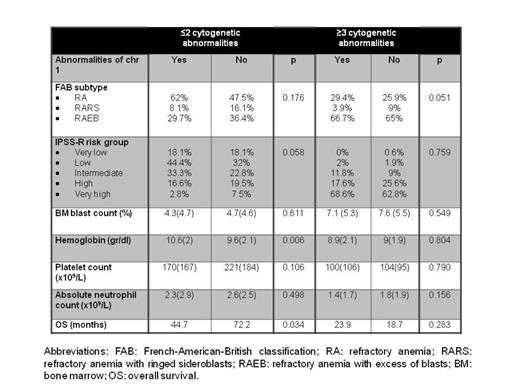
According to the number of cytogenetic abnormalities, translocation (43.2%) was the most frequent cytogenetic abnormality observed in the group of ≤2 abnormalities and chr 1 involvement (group 1), becoming chr 7 (16.2%) the most recurrently affected. However, deletion (24.5%) predominated in the group of ≥ 3 abnormalities and chr 1 involvement (group 2). In the first group, long arm was more frequently involved (48.6%) whilst both arms were involved in only 5.5% of cases, being this condition more common in the second group. Moreover, the short arm was mostly restricted to the second group (32.1%). In the first group, chr 5 and chr 7 were affected in 8.1% and 18.9% of cases, respectively, compared to group 2 (67% and 39.6%, respectively). A higher hemoglobin level was observed in the first group (10.6 vs. 9.6 g/dl; p=0.006). However, we observed no differences in terms of bone marrow blasts, platelet count and absolute neutrophil count between these two groups (table 1).
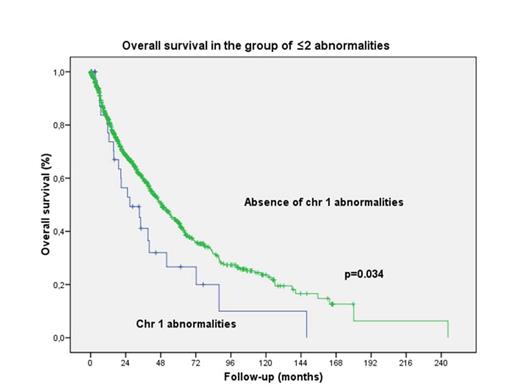
The median survival was significantly lower in the group with chr 1 involvement (34.1 vs. 64.7 months; p<0.001). When patients were classified attending to the number of abnormalities, the prognostic impact of chromosome 1 was restricted to the group with ≤2 abnormalities (44.7 vs. 72.2 months; p=0.034) (figure 1). However, we observed no differences in terms of survival in the group with ≥ 3 abnormalities (24 vs. 19 months; p=0.283) (table 1). Transformation to acute myeloid leukemia (AML) was observed in 35.6% of patients with chr 1 involvement, in comparison to the 20.2% of the control group (p=0.001).
CONCLUSIONS: Chr 1 involvement in patients with MDS is more frequently associated with complex karyotype, generally with chr 5 and 7 additionally involved and a low platelet count. In those patients carrying a complex karyotype, the presence of chromosome 1 does not provide additional prognostic information. However, in the group of patients with ≤ 2 abnormalities, chr 1 aberrations are associated with a significant reduced OS, suggesting that those should be included in the high risk cytogenetic group.
Acknowledgments: Ministerio de Sanidad y Consumo, Spain (PI 11/02010); Red Temática de Investigación Cooperativa en Cáncer (RTICC, FEDER) (RD12/0036/0044); 2014 SGR225 (GRE) Generalitat de Catalunya,Fundació Internacional Josep Carreras, Obra Social “la Caixa” y de Celgene (España).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal