Abstract
BACKGROUND
Most patients with chronic phase (CP) chronic myeloid leukemia (CML) are successfully treated with tyrosine kinase inhibitors (TKIs) targeting ABL1. Despite the good results, TKI treatment rarely results in cure, and some patients relapse and progress to advanced phases of CML. Accelerated phase and blast crisis (BC) have remained a therapy challenge. We set out to identify novel candidate drugs for chronic and advanced phase CML by using an unbiased high-throughput drug testing platform and utilizing both primary patient cells (CP and BC) and cell lines.
METHODS
CML BC cell lines used: K562 (erythroleukemic), MOLM-1 (megakaryocytic) and EM-2 (myeloid). Primary bone marrow (BM) and peripheral blood (PB) samples were derived from 3 CML patients with BC, two of which were TKI-resistant. Patient 1 had developed resistance to imatinib and nilotinib due to an E274K mutation in ABL1 kinase domain, whereas patient 2 was resistant to imatinib, nilotinib, and dasatinib due to a T315I mutation. In addition to BC patients, samples from 23 newly diagnosed CML CP patients were screened. BM cells from 4 healthy individuals were used as controls. Functional profiling of drug responses was performed with a high-throughput drug sensitivity and resistance testing (DSRT) platform comprising 306 anti-cancer agents. Cells were dispensed to pre-drugged 384-well plates and incubated for 72 h. Cell viability was measured using a luminescence cell viability assay (CellTiter-Glo, Promega). A Drug Sensitivity Score (DSS) was calculated for each drug using normalized dose response curve values. The drug sensitivities of the primary cells were further normalized against the median values from healthy controls, resulting in leukemia-specific sensitivity scores (sDSS).
RESULTS
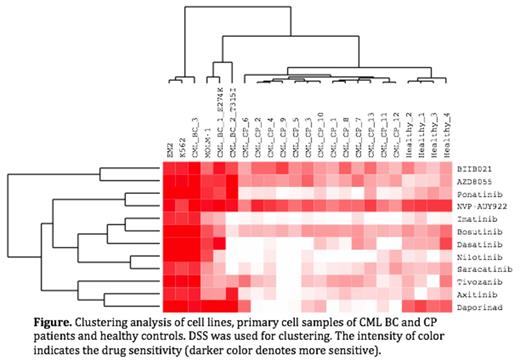
Drug sensitivities of CML cell lines correlated closely (EM-2 vs. K-562, rS=0.89; EM-2 vs. MOLM-1, rS=0.82; K-562 vs. MOLM-1, rS=0.78; p<0.0001 for all correlations). Similarly, patient samples had good correlation with cell line samples (rS=0.82 based on median values; p<0.0001). The cell lines were highly sensitive to ABL1-targeted TKIs, with the exception of the MOLM-1, which showed only modest sensitivity (Figure). The clinically TKI-resistant patient samples were also resistant to BCR-ABL1 inhibitors ex vivo (e.g. T315I sensitive only to ponatinib), further validating the DSRT assay data. Other drugs that exhibited high DSS in the CML cell lines and high sDSS in the BC patient samples included mTORC1/2 inhibitors (e.g. AZD8055, AZD2014, INK128), HSP90 inhibitors (e.g. NVP-AUY922, BIIB021) and a NAMPT inhibitor daporinad. Remarkably, the DSRT results from newly diagnosed CML CP differed clearly from those derived from the cell line and CML BC samples. In the clustering analysis, CML BC and cell line samples clustered together, whereas CML CP samples formed a separate group (Figure). The leukemia-specific scores were generally much lower in CML CP samples, which made identifying novel candidate compounds challenging. Most surprisingly the responses to TKIs were practically nonexistent in CML CP samples. CP TKI insensitivity was further assessed with primary cells sorted in CD34pos and CD34neg fractions. Preliminary results from two patients suggested that CD34pos cells were more sensitive to TKIs when compared to CD34neg or whole mononuclear fraction.
CONCLUSIONS
DSRT is a powerful platform for identifying novel candidate molecules for CML BC patients. Our results indicate that mTORC1/2 inhibitors (such as AZD8055, or AZD2014), HSP90 (such as NVP-AUY922/luminespib) and NAMPT inhibitors in particular warrant further clinical evaluation. TKI-insensitivity of CML CP samples suggests that the survival of mature myeloid cells in vitro is not BCR-ABL1 dependent and reflects a clear biological difference between CP and BC patient cells.
Kallioniemi:Medisapiens: Consultancy, Membership on an entity's Board of Directors or advisory committees. Mustjoki:Bristol-Myers Squibb: Honoraria, Research Funding; Novartis: Honoraria, Research Funding. Porkka:Bristol-Myers Squibb: Honoraria, Research Funding; Novartis: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal