Abstract
Introduction: Multiple myeloma (MM) remains an incurable disease in need of new therapies with unique targets. Ibrutinib is a first-in-class, once-daily, oral, covalent inhibitor of Bruton’s tyrosine kinase (BTK), an essential enzyme in the B-cell receptor signaling pathway. While BTK is essential for the development and function of B cells and is down-regulated in plasma cells, the expression of BTK in malignant plasma cells is increased 4-fold and comparable to BTK expression levels in chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL). In addition, pre-clinical models show that BTK inhibition with ibrutinib led to direct inhibition of both osteoclast bone resorption and the release of osteoclast-derived tumor growth factors (Tai et al, Blood 2012). Taken together these data suggest that ibrutinib may have a role in the treatment of MM.
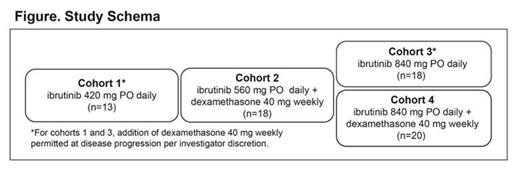
Methods: This open label phase 2 dose escalation study was designed to enroll patients in 4 cohorts (Figure) to evaluate efficacy (≥MR) and secondary endpoints of safety, PK, ORR and DOR. Patients must have had documented non-responsive/progressive disease at the time of study entry following at least 2 prior lines of therapy including at least one immunomodulatory agent. Efficacy and safety were assessed at 4 weeks intervals using the IMWG response criteria for efficacy assessments (Rajkumar et al, Blood 2011), while safety was assessed according to CTCAE v4.0 criteria.
Results: As of 15 May 2014 and a median follow up of 15.2 months, 69 patients with a median age of 64 years (range 43-81) were dosed, of which 20% had either a del 17p or p53 deletion. The number of median prior therapies was 4 (range, 2-14), 41% had ≥ 5 prior therapies and 80% had undergone autologous stem cell transplant. Sixty-two percent of patients were refractory to their last line of therapy and of the 65 patients that had received prior therapy with both an immunomodulatory agent and a proteasome inhibitor, 44% were refractory to both.
Anti-tumor activity was noted across all cohorts. The highest activity with a clinical benefit rate (CBR) of 25% including 1 PR, 4 MR and 5 sustained (>4 cycles) SD was observed in Cohort 4. (Table) This led to expansion of Cohort 4 per protocol design. In Cohorts 1 and 3, 14 patients had dex added following PD, resulting in 1 PR and 9 SD.
Overall, 57% experienced a Grade 3 or higher adverse event. The most commonly reported non-hematologic toxicities (any grade) were diarrhea (51%), fatigue (41%), nausea (35%), dizziness (25%), and muscle spasms (23%). The majority were Grade 1 and 2. Myelosuppression had a reported overall incidence of any grade anemia (29%), thrombocytopenia (23%), and neutropenia (7%) with 16%, 9% and 4% being Grade 3, respectively. There were no clinically meaningful differences among dose levels. Twenty-three patients experienced a SAE for a total of 47 reported events with 16 assessed as possibly/definitely related to ibrutinib per investigator. At least one dose modification occurred in 22% of patients, with 6 discontinuing due to an adverse event.
At the time of the data cut-off 7 patients remain on study treatment. The most common reason for treatment discontinuation was PD in 47% of patients, with additional patients discontinuing due to investigator discretion (18%), patient decision (7%) and non-compliance (3%).
Conclusions: In this heavily pre-treated patient population ibrutinib, as a single agent and in combination with dex, demonstrated evidence of anti-tumor activity. There was a trend toward improved efficacy (≥MR) in Cohort 4 and treatment was well tolerated with manageable toxicities. Ongoing correlative studies are being conducted to determine changes in cytokines, chemokines and indices of bone metabolism and to determine the effect of dex, a known CYP3A4/5 inducer, on the pharmacokinetic profile of ibrutinib. In addition, ibrutinib is currently being evaluated in combination with carfilzomib in an ongoing Phase1/2b study. (NCT01962792)
Confirmed Response by Assigned Treatment
| . | Cohort . | |||
|---|---|---|---|---|
| Response, n (%) . | 1 (n=13) . | 2 (n=18) . | 3 (n=18) . | 4 (n=20) . |
| PR | 1 | 1 | - | 1 |
| MR | 1 | - | - | 4 |
| SD ≥ 4 cycles | 2 | 4 | 6 | 5 |
| SD < 4 cycles | 5 | 6 | 4 | 1 |
| PD | 4 | 5 | 7 | 5 |
| Not evaluable | - | 2 | 1 | 4 |
| . | Cohort . | |||
|---|---|---|---|---|
| Response, n (%) . | 1 (n=13) . | 2 (n=18) . | 3 (n=18) . | 4 (n=20) . |
| PR | 1 | 1 | - | 1 |
| MR | 1 | - | - | 4 |
| SD ≥ 4 cycles | 2 | 4 | 6 | 5 |
| SD < 4 cycles | 5 | 6 | 4 | 1 |
| PD | 4 | 5 | 7 | 5 |
| Not evaluable | - | 2 | 1 | 4 |
Not evaluable – no post-baseline assessments
Off Label Use: Discussion of efficacy and safety data with ibrutinib as single-agent and in combination with dexamethasone in patients with relapsed and relapsed/refractory multiple myeloma treated in a phase 2 clinical trial. Huff:Celgene, Millenium: Consultancy. Bensinger:Pharmacyclics, Novartis, Celgene, Millenium, Sanofi, Acetylon: Consultancy, Research Funding. Siegel:Celgene, Millennium, Onyx: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Jagannath:Celgene, BMS, Jansen, Sanofi-Aventis: Honoraria. Lebovic:Onyx, Celgene: Speakers Bureau. Anderson:Celgene, Millenium, Onyx, : Speakers Bureau. Elias:Pharmacyclics, Inc.: Employment. Clow:Pharmacyclics, Inc.: Employment. Fardis:Pharmacyclics: Employment. Graef:Pharmacyclics: Employment. Bilotti:Pharmacyclics: Employment. Richardson:Celgene, Millennium, Johnson&Johnson: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal