Abstract
Introduction:
DLBCL is the more common non Hodgkin lymphoma. This is an aggressive lymphoma that is treated with a standard chemotherapy regimen: R-CHOP. In the last years attempts have been done to improve the outcome both increasing dose-density (CHOP14) or intensity (CHOEP, ACVBP, autologous stem cell transplantation) without obtaining benefit in terms of survival. This has allowed setting R-CHOP administered every 21 days (R-CHOP21) as the standard treatment for DLBCL patients.
RDI is an important issue to consider when treating malignancies. Although this a well-known prognostic factor in Hodgkin lymphoma, scarce information has been published in DLBCL.
Objective:
The purpose of this study is further analyzing the prognostic impact of RDI in two cohorts of DLBCL patients treated with R-CHOP21 or R-CHOP14, to evaluate its differential impact when increasing dose density.
Material and methods:
All patients diagnosed of DLBCL from January-1999 to June-2013 at University Hospital Son Espases were retrospectively identified from Pathology Department registry to avoid selection bias. Only patients treated with R-CHOP21 or R-CHOP14 +/- radiotherapy were included (N=115). To increase the R-CHOP14 cohort we added also all patients treated with R-CHOP14 in the same time period in two additional hospitals (Hospital Son Llatzer of Palma and Hospital del Mar of Barcelona) identified from their Pharmacy registries to avoid selection bias (N=42). Other regimes, consolidations or maintenance were excluded. Table 1 shows main characteristics of the global series (N=157).
RDI represents the ratio of the amount of a drug actually administered to the amount planned for a fixed time period. RDI was calculated as previously described. Briefly, RDI of each drug was obtained followed by an average of RDI in CHOP consisting in the sume of RDI of the 3 drugs divided by 3.
Main prognostic factors at diagnosis in DLBCL were obtained, including international prognostic index (IPI) factors. Evaluations were carried out following standard guidelines.
Results:
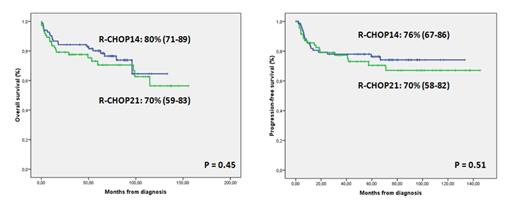
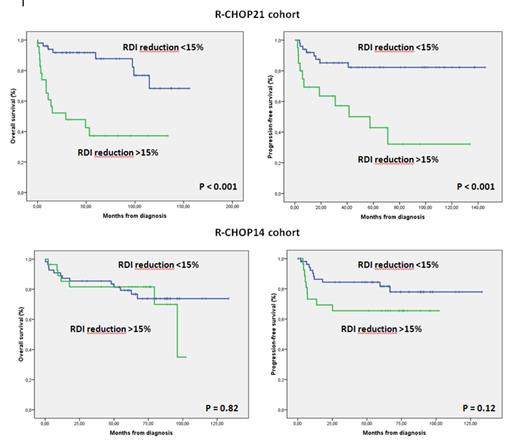
Overall response and complete response rates were similar in both groups:86% and 76% for R-CHOP21 and 94% and 74% for R-CHOP14(p=0.17 and p=0.85, respectively). Median follow-up for alive patients was 68 months (4-156). There were no differences between the two cohorts in terms of either OS or PFS (Figure 1). In the R-CHOP21, both a reduction higher than 15% in RDI [RR 7.41 (2.51-21.83); (p<0.001)] and an unfavorable R-IPI [RR 2.99 (1.1-8.16); (p=0.032) were independently associated with a worse OS. For PFS only a reduction higher than 15% in RDI [RR 4.41 (1.77-10.99) (p=0.001) was independently associated to worse PFS. By contrast, in the R-CHOP14 group an unfavourable NCCN-IPI [RR 8.74 (2.23-34.25); (p=0.002)] and the presence of B-symptoms [RR 5.13 (1.98-13.3); p=0.001)] was independently associated to worse OS and having a AA stage III-IV [RR 5.09 (1.14-22.62); p=0.032)] and bulky disease [RR 3.95 (1.46-10.7); p=0.007)] were independently related to worse PFS. RDI reductions did not show any significant impact in OS or PFS in patients treated with R-CHOP14 (Figure 2).
Conclusions:
Overall in our series there were no differences in terms of response or survival between patients treated with R-CHOP21 or R-CHOP14. A higher rate of RDI reduction was observed in the R-CHOP14 group. However, the impact of RDI reductions on response and survival was only observed in the R-CHOP21 group but not in patients treated with R-CHOP14. We can conclude that R-CHOP21 and R-CHOP14 are equivalent regimens in terms of response and survival only if RDI reductions are avoided. For patients receiving R-CHOP21 we recommend using clinical and support measures in order to avoid RDI reductions.
Main clinical characteristics of the patients.
| . | R-CHOP21 group (n=74) . | R-CHOP14 group (n=83) . | P . |
|---|---|---|---|
| Age (median & range) | 65 (25-88) | 55 (15-79) | 0.005 |
| Sex (M/F) | 34 (46%) / 40 (54%) | 51 (61%) / 32 (39%) | 0.056 |
| ECOG PS > 1 | 17 (23%) | 18 (22%) | 0.85 |
| Ann Arbor stage III-IV | 40 (54%) | 48 (58%) | 0.75 |
| B-symptoms | 25 (34%) | 26 (31%) | 0.86 |
| Elevated LDH | 33 (46%) | 40 (49%) | 0.75 |
| > 1 extranodal site | 8 (11%) | 19 (23%) | 0.057 |
| Bulky disease | 23 (31%) | 34 (41%) | 0.24 |
| R-IPI unfavorable | 24 (32%) | 26 (32%) | 1 |
| NCCN-IPI: - Low - Low-intermediate - High-intermediate - High | 9 (13%) 27 (39%) 26 (38%) 7 (10%) | 17 (21%) 35 (44%) 24 (30%) 4 (5%) | 0.31 |
| Elevated Beta-2-microglobulin | 32 (49%) | 31 (39%) | 0.24 |
| Radiotherapy | 27 (36%) | 27 (32%) | 0.62 |
| . | R-CHOP21 group (n=74) . | R-CHOP14 group (n=83) . | P . |
|---|---|---|---|
| Age (median & range) | 65 (25-88) | 55 (15-79) | 0.005 |
| Sex (M/F) | 34 (46%) / 40 (54%) | 51 (61%) / 32 (39%) | 0.056 |
| ECOG PS > 1 | 17 (23%) | 18 (22%) | 0.85 |
| Ann Arbor stage III-IV | 40 (54%) | 48 (58%) | 0.75 |
| B-symptoms | 25 (34%) | 26 (31%) | 0.86 |
| Elevated LDH | 33 (46%) | 40 (49%) | 0.75 |
| > 1 extranodal site | 8 (11%) | 19 (23%) | 0.057 |
| Bulky disease | 23 (31%) | 34 (41%) | 0.24 |
| R-IPI unfavorable | 24 (32%) | 26 (32%) | 1 |
| NCCN-IPI: - Low - Low-intermediate - High-intermediate - High | 9 (13%) 27 (39%) 26 (38%) 7 (10%) | 17 (21%) 35 (44%) 24 (30%) 4 (5%) | 0.31 |
| Elevated Beta-2-microglobulin | 32 (49%) | 31 (39%) | 0.24 |
| Radiotherapy | 27 (36%) | 27 (32%) | 0.62 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal