Abstract
Allogeneic stem cell transplantation (SCT) is widely used as post-remission treatment in younger patients with poor or intermediate risk AML. Transplant decisions are mainly based on cytogenetic and molecular risk group, age, comorbidity and on the availability of a suitable donor. Secondary AML, including therapy-related AML (t-AML) and AML after an antecedent hematological disorder (AHD-AML), constitutes more than one fourth of the AML cases and is a predictor of a poor outcome. However, the extent to which SCT improves outcome of this patient group is poorly studied.
In this study, we set out to investigate the role of SCT for the survival of secondary AML patients within the population-based Swedish Adult Acute Leukemia Registry. In total, 5881 patients with AML diagnosed during the period 1997 – 2013 were included in the study. Of these, 4233 (72%) were de novo AML, 1098 (19%) AHD-AML and 550 (9%) t-AML. The median age at diagnosis was 70 in de novo AML, 73 in AHD-AML and 70 in t-AML. The gender distribution was equal in de novo AML (51% males). In AHD-AML, there was a male predominance of 57% whereas in t-AML, there was a female predominance of 56%. The proportion of patients who underwent SCT in first remission (CR1) was 10% in de novo AML, 5% in AHD-AML and 8% in t-AML (de novo vs AHD-AML p < 0.001, de novo vs t-AML p = 0.068, AHD-AML vs t-AML p = 0.081; Fisher's exact test). In patients aged 65 or below, the proportion of SCT in CR1 was 24%, 21% and 20%, respectively. The median age of SCT patients was 48 (range 17 – 71) in de novo AML, 57 (27 – 76) in AHD-AML and 49.5 (18 – 68) in t-AML. In de novo AML, the distribution of genetic risk groups among SCT patients was 3% low risk, 55% intermediate risk and 42% high risk. Corresponding figures for AHD-AML was 0%, 34% and 66% and for t-AML 5%, 45% and 50% respectively (de novo vs AHD-AML p = 0.004, de novo vs t-AML p = 0.299, AHD-AML vs t-AML p = 0.124; Fisher's exact test).
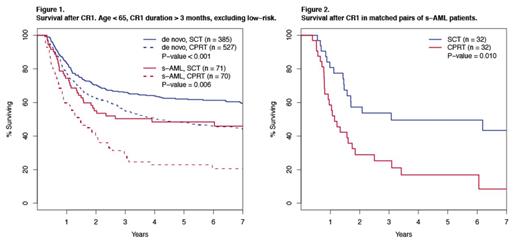
The estimated median survival after the date of SCT in CR1 was 15 months in AHD-AML and 22 months in t-AML but not reached in de novo AML (95% lower confidence limit 107 months). Among patients <65 years who had been in CR for 3 months (genetic low risk excluded), those with secondary AML had a greater benefit from consolidation with SCT than those with de novo AML (Figure 1). The projected 7-year survival in de novo AML was 60% with SCT and 44% with conventional post remission therapy (CPRT) as compared to 46% and 21%, respectively, in secondary AML. The survival hazard with SCT was 0.45 in secondary AML (95% CI 0.28-0.72) as compared to 0.66 in de novo AML (CI 0.53 – 0.82), by multivariable Cox regression adjusting for type of secondary AML, age, sex, and cytogenetic risk group. To refine the analysis correcting for major confounding factors, a matched pair analysis was performed in patients with CR longer than 3 months. Matching criteria were type of secondary AML (AHD or t-AML), cytogenetic risk group and age (+/- 3 years). Remission of the patient with CPRT was at least as long as the time between CR1 and transplantation for the matched patient undergoing SCT. The projected 7-year survival rate was 43% in the SCT and 8% in the CPRT group (p = 0.01; log-rank test, Figure 2) further indicating a benefit for SCT as post remission therapy in secondary AML. We conclude that SCT improves survival in patients with secondary AML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal