Abstract
Angiogenesis is a complicated process involving endothelial proliferation, migration, and finally formation of functional vessels, in which perivascular cells play assistant roles. Mesenchymal stem cells (MSCs) from distinct human tissues have been proved to share functional properties and gene-expression profile with perivascular cells and to be proangiogenic. In this study we compared the proangiogenic ability of three types of MSC derived from human adipose stromal cells (ADSCs), umbilical cord (UCMSCs) and endometrium (EMSCs).
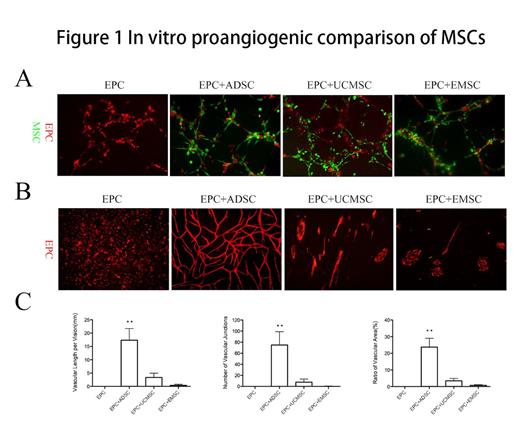
Three types of MSCs all located around the tubular like structures formed by EPCs in coculture system on Matrigel in vitro (Figure 1A). However, different MSCs showed different potential for stimulating vessel formation of EPCs. After 6 days' coculture, we found that EPCs seeded on ADSCs monolayer formed more organized capillary-like network (Figure 1B, P<0.01), and the length of vascular, number of junctions and ratio of vascular area was 18.96±3.52, 81.72±14.09 and 23.97%±2.11%, respectively (Figure 1C). EPCs seeded on UCMSCs only formed single tube-like structure (length, 2.90±1.31; junctions, 6.94±3.22; area, 3.05%±1.29%), while EPCs seeded on EMSCs gathered together not to form capillary-like structure (Figure 1B, C).
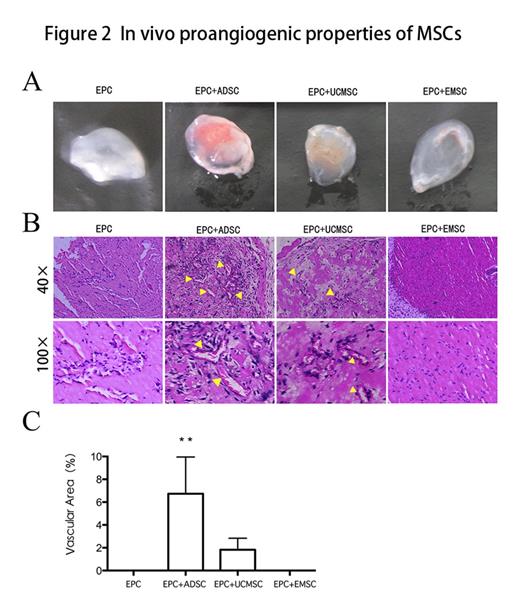
Furthermore, we compared their proangiogenic potential of three types of MSCs. Matrigel contained MSCs and EPCs (ratio 3:2, total 2*106) was injected into nude mouse dorsal subcutaneous. 7 days following the injection, Matrigel was stripped off for the analysis of microvessels. As shown in Figure 2, three types of MSCs all promoted the formation of new microvessels. ADSC had the strongest stimulating effects, and formed more microvessels containing a large number of erythrocytes as shown by the appearance and HE staining (6.43%±2.57%). However, microvessel structures were not observed in the matrigel containing EPCs alone.
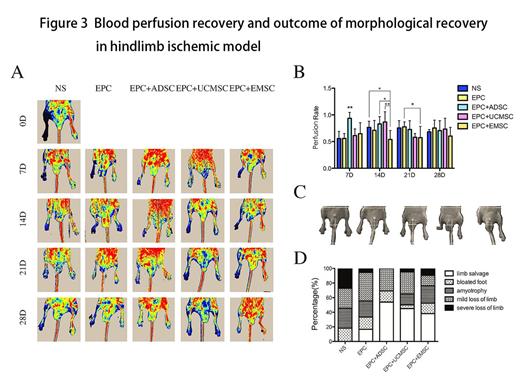
Moreover, we assessed the therapeutic effects of co-transplantation of EPCs and MSCs in mouse hindlimb ischemic model. Right femoral artery ligation and excision was performed on anesthetized nude mice. After 24h of surgery, EPCs and MSCs were co-transplanted by tail intravenous injection (n=5, total 6.25*105; MSC/EPC ratio, 3:2). Blood flow of the ischemic limb was measured at 0, 7, 14, 21, 28 days after cell transplantation using Laser Doppler Perfusion Imager (Figure 3A). The results showed that the co-transplantation of EPCs with ADSCs significantly improved blood flow of ischemic limb after day 7 of transplantation (0.94±0.10, P<0.01, Figure 3B), and the final limb salvage rate in mice was significantly raised after day 28 of transplantation (Figure 3C, D). Thus, the blood stream reconstitute in early stage is the key factor for the final outcome of ischemic limb.
We queried whether the different stimulation effects of MSCs on the vessel formation of EPCs are caused by MSC-secreted proangiogenic cytokines. Firstly, we analyzed the effects of MSC-CM on the proliferation and migration of EPCs in vitro, and found that migration rates/numbers of EPCs was highly increased by ADSC-CM (69.52%±9.66%, P<0.05) compared with UCMSC-CM and EMSC-CM. Next, we analyzed proangiogenic cytokines in MSC-CM using cytokine antibody array. The results showed that ADSCs secreted more proangiogenic cytokines such as VEGF-A, HGF, PDGF-BB and bFGF, and less inhibitor such as thrompospondin-1 in comparision to UCMSCs and EMSCs.
In conclusion, MSCs could promote the formation of new microvessles of EPCs, and ADSCs are more efficient than UCMSCs or EMSCs by secreting more proangiogenic cytokines and less inhibitor. Thus ADSCs may be an ideal cellular source for the treatment of ischemia vascular disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal