Abstract
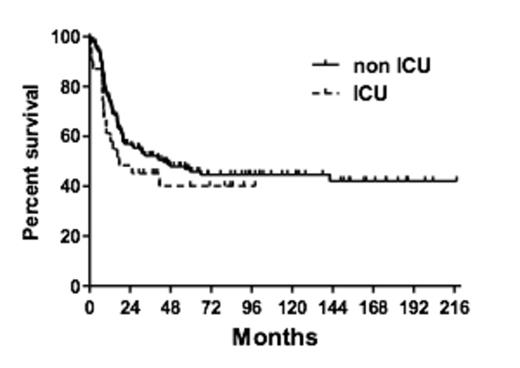
Acute lymphocytic leukemia (ALL) and Burkitt lymphoma (BL) are highly aggressive hematologic neoplasms. We analyzed reasons for and the incidence of admission to the intensive care unit (ICU) in de novo ALL/BL patients (pts) as well as their ICU and long-term outcome. A total of 177 consecutive pts (age 15-88 years, f/m ratio 1:1.3), including 135 with ALL (B-ALL, n=12; c-ALL, n=26; prae-B-ALL, n=33; T-ALL, n=28; bcr/abl+ ALL, n=29; T-LBL, n=3; ALL NOS, n=4) and 42 with BL were analyzed retrospectively. First-line chemotherapy (CHT) was administered between 02/1995 and 01/2013 according to the Hšlzer-protocol. In a subset of patients (n=52) hematopoietic stem cell transplantation (HSCT) was performed in complete remission (CR). Thirty-one pts (17.5%) required intensive care, 21 (11.9%) during induction CHT, 6 (3.4%) during conventional post-remission therapy and 4 (2.3%) within one year after HSCT in first CR. In these 31 pts the reasons for ICU admission were «observation after surgery due to malignancy«, therapy-related complications (n=10, 32%), respiratory failure (n=8, 26%), sepsis (n=4, 13%), neurological deterioration (n=3, 10%), renal failure (n=3; 6%) as well as cardiopulmonary resuscitation, bleeding, III¡ AV-blockage and pancreatitis in one patient each. The percentage of ICU admissions was comparable in BL (23%) and ALL (16%; p=0.26). In BL more pts were admitted to the ICU for observation after surgery (50%) compared to ALL patients (23%; p=0.15). Whereas intensive care was required in pts with BL only during the induction phase of CHT (Block A1), ALL pts were admitted during induction as well as during post-remission treatment (conventional CHT or HSCT; p<0.05). At ICU admission the median SAPS II score in all pts was 45 (range 13-93). Invasive mechanical ventilation was necessary in 28 pts (90%) and vasopressor therapy in 29 pts (94%). The median number of days at the ICU was 6 (range 1-88 days) and 25/31 pts (81%) were ICU survivors. All pts with BL (n=10) survived the ICU, and 71% of our ALL patients (15/21, p=0.06) were ICU survivors. In ICU pts, the medin survival from hospital admission was 18 months and thus shorter compared to non-ICU pts (44 months) with a similar plateau at 60 months of 40% and 43%, respectively (Figure 1). However, these differences were not statistically significant (p=0.32). Moreover, no differences in the median survival were observed with regard to continuous complete remission (CCR). In summary, a substantial number (17.5%) of pts with ALL/BL require intensive care during first line CHT. Importantly, the long-term survival and CCR of the ICU pts did not differ significantly from that of non-ICU pts. These observations have obvious clinical implications and are in favor of ICU admission and intensive care as needed in this group of aggressive malignancies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal