Abstract
Background: Double-unit cord blood transplantation (DCB-T) is a rapidly available alternative to unrelated donor transplantation (URD-T) for patients with high-risk acute leukemia or advanced CML. Retrospective analyses in adult DCB-T suggest that double-unit CB grafts may be associated with improved disease-free survival (DFS). However, the prioritization of URD-T vs DCB-T is controversial.
Methods: We evaluated 175 consecutive adult allograft recipients (120 URD-T and 55 DCB-T) aged 16-60 years transplanted 10/2005-11/2012 for acute leukemia in morphologic remission or aplasia (113 AML/ biphenotypic, 50 ALL), or advanced CML (n = 12). URD grafts were 7-8/8 HLA-matched (74 8/8, 46 7/8). CB grafts were 4-6/6 donor-recipient HLA-matched (4 6/6, 51 5/6, 55 4/6). All patients received either high dose or reduced intensity myeloablative conditioning. The majority of URD-T recipients (n = 111, 93%) received T-cell depleted (TCD) grafts with rabbit ATG, whereas GVHD prophylaxis for DCB-T was calcineurin-inhibitor/mycophenolate mofetil.
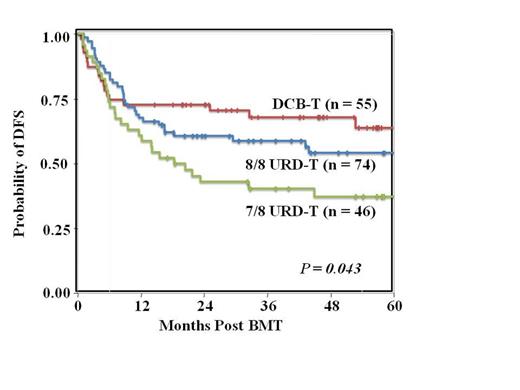
Results: The median ages of URD-T (43 years) and DCB-T (42 years) recipients were similar (p = 0.713). Distributions of gender, recipient CMV positivity, HCT-CI scores, time from diagnosis or relapse to transplant, diagnoses, disease risk, and percentage of patients with minimal residual disease pre-transplant were also similar. Neutrophil engraftment was slower in DCB-T (95%, median 24 days) than URD-T (100%, median 11 days) (p <0.001). While the incidence of grade II-IV acute GVHD at day 100 was lower in TCD URD-T recipients (15%) than in unmodified URD-T (56%) and DCB-T (55%), p = 0.002, the incidence of day 100 grade III-IV acute GVHD was similar in TCD URD-T, unmodified URD-T, and DCB-T recipients (p = 0.794). With a comparable survivor follow-up [URD-T median 51 months (range 15-99) vs DCB-T median 46 months (range 15-92)], transplant-related mortality was similar (3-year estimates: URD-T 25% vs DCB-T 24%, p = 0.838) whereas the relapse risk was decreased after DCB-T (3-year estimates: URD-T 23% vs DCB-T 9%, p = 0.008). Overall, the 3-year DFS after URD-T was 52% and 68% after DCB-T (p = 0.056). When split into 3 groups, the 3-year DFS was 59% in 8/8 URD-T, 40% in 7/8 URD-T, and 68% in DCB-T, p = 0.043 (Figure). Multivariate analysis was performed to determine risk factors for disease relapse or death in the 175 patients (Table). Female gender (HR 1.65, p = 0.029), diagnosis of ALL (HR 2.11, p = 0.002), and mismatched URD-T (HR 1.97, p = 0.027) were each significantly associated with treatment failure.
Conclusions: DCB-T can achieve favorable DFS in adults with acute leukemia and CML with low relapse rates. In this series, multivariate analysis demonstrated that mismatched URD-T was independently associated with lower DFS. Our findings support use of DCB-T as an immediate alternative for high-risk acute leukemia and advanced CML in adult patients without a readily available 8/8 allele HLA-matched unrelated volunteer donor. This could have the additional benefit of speeding time to transplant in high-risk patients.
| Variable . | Multivariate HR (95% CI) . | P-value . |
|---|---|---|
| Male Female | Reference 1.65 (1.05-2.59) | 0.029 |
| Recipient CMV Negative Recipient CMV Positive | Reference 1.34 (0.85-2.12) | 0.201 |
| HCT-CI score 0-2 HCT-CI score > 3 | Reference 1.56 (0.98-2.47) | 0.059 |
| AML/CML ALL | Reference 2.11 (1.30-3.41) | 0.002 |
| DCB-T 8/8 URD-T 7/8 URD-T | Reference 1.32 (0.72-2.41) 1.97 (1.08-3.60) | - 0.365 0.027 |
| Variable . | Multivariate HR (95% CI) . | P-value . |
|---|---|---|
| Male Female | Reference 1.65 (1.05-2.59) | 0.029 |
| Recipient CMV Negative Recipient CMV Positive | Reference 1.34 (0.85-2.12) | 0.201 |
| HCT-CI score 0-2 HCT-CI score > 3 | Reference 1.56 (0.98-2.47) | 0.059 |
| AML/CML ALL | Reference 2.11 (1.30-3.41) | 0.002 |
| DCB-T 8/8 URD-T 7/8 URD-T | Reference 1.32 (0.72-2.41) 1.97 (1.08-3.60) | - 0.365 0.027 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal