Abstract
Introduction: Several studies have suggested that umbilical cord blood transplantation (UCBT) is associated with a lower risk of relapse when compared to matched and mismatched unrelated donor transplants (URD). However, the impact of minimal residual disease (MRD) on risk of relapse has not been investigated in comparative studies. With the aim to compare relapse and other transplantation outcomes based on MRD status at time of transplant, we conducted a retrospective analysis comparing myeloablative UCBT to URD.
Methods: Between January 2006 and December 2012, 566 patients underwent a first allogeneic hematopoietic cell transplantation for hematologic malignancies with either a cord blood (CB) or URD stem cell graft. The UCBT group (n=112) received either a single- or double-unit CB graft. In the URD group (n=447), patients were allele-level matched with the donor at HLA-A, -B, -C, -DQB1, and -DRB1 (MURD (10/10), n=332) or mismatched for a single allele (MMURD (9/10), n=115). All patients received a myeloablative conditioning regimen. Graft–versus–host disease prophylaxis (GVHD) consisted of a calcineurin inhibitor (cyclosporine or tacrolimus) and either methotrexate (MURD and MMURD) or mycophenolate mofetil (UCBT). Ten-color multiparameter flow cytometry (MFC) studies on bone marrow aspirates were performed before HCT to evaluate MRD. Any level of residual disease was considered MRD-positive. The cause-specific hazards of failure (for death and for relapse) were compared between the UCBT group and each of the MRD groups using Cox regression.
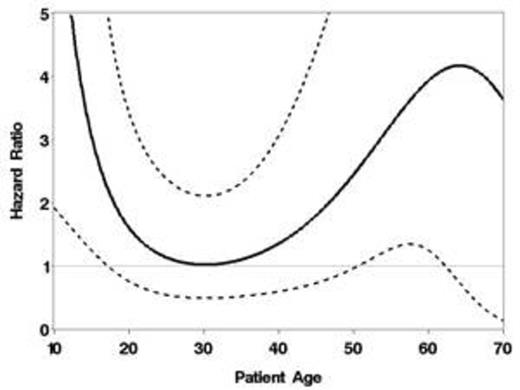
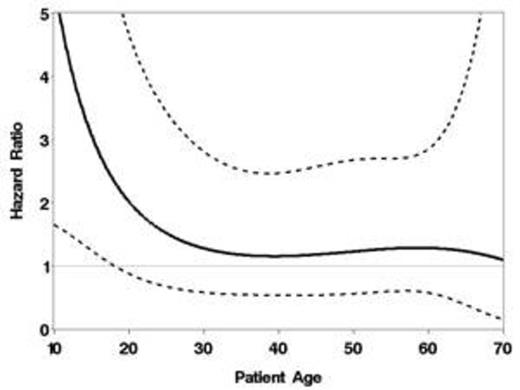
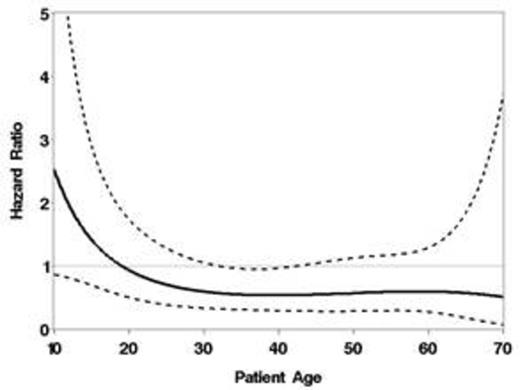
Results Recipients of UCBT were younger than MMURD and MURD, more likely to be non-caucasian, and more likely to be CMV seropositive. The UCBT and MMURD groups had a higher proportion of patients with higher disease risk when compared to MURD. MRD-positive patients were 34 (30%), 122 (36%) and 44 (38%) for UCBT, MURD and MMURD, respectively. The hazard of relapse in the MMURD group was higher than that in the UCBT group after adjusting for age, disease severity, year of HSCT, and MRD (HR=2.27; 95% CI 1.10-4.67; p=.03). The adjusted relative hazard of relapse in the MURD compared to the UCBT group depended on age (p=.03, interaction test), with younger and older patients having an increased risk and all other patients having a similar risk (Figure 1). The adjusted relative hazard of overall mortality (OM) in the MMURD group compared to the UCBT group was suggestively different based on MRD status with a HR=1.96 (95% CI 0.94-4.08; p=0.07) in MRD-positive patients and HR=1.00 (95% CI 0.54-1.83; p=0.99) among MRD-negative patients. With respect to the MURD group as compared to the UCBT group, the adjusted relative hazard was dependent on both MRD status and age. These associations are shown in Figures 2a (MRD-positive) and 2b (MRD-negative), with an increased hazard in younger MRD-positive patients and perhaps decreased hazard among older MRD-negative patients. The hazard of relapse was higher among MRD-positive patients than that among MRD-negative patients, but only in the MMURD (adjusted HR=1.83; 95% CI 1.05-3.19; p=0.03) and MURD group (adjusted HR=1.83; 95% CI 1.22-2.74; p=0.003). In stark contrast, the risk of relapse was similar between MRD-positive and MRD-negative patients in the UCBT group (HR=0.96; 95% CI 0.44-2.07; p=.91).
Conclusions: Contrary to what has been demonstrated previously in MURD and MMURD transplants, our results suggest that pre-transplant MRD is not associated with increased risk of relapse after myeloablative UCBT. The data also suggest that the risk of relapse was higher in MMURD and was dependent on age for MURD recipients when compared to UCBT. The observed lower risk of relapse and the lack of impact of pre-transplant MRD in UCBT recipients suggest that UCBT should be considered first in younger patients with hematologic malignancies at high risk of relapse who lack an HLA-matched sibling donor.
Hazard ratio (solid line) for relapse (MURD vs. UCBT) as a function of age. Dotted lines represent pointwise 95% confidence limits.
Hazard ratio (solid line) for relapse (MURD vs. UCBT) as a function of age. Dotted lines represent pointwise 95% confidence limits.
A) Hazard ratio (solid line) for overall mortality (MURD vs. UCBT) as a function of age among MRD-positive patients (A) and MRD-negative patients (B). Dotted lines represent pointwise 95% confidence limits.
A) Hazard ratio (solid line) for overall mortality (MURD vs. UCBT) as a function of age among MRD-positive patients (A) and MRD-negative patients (B). Dotted lines represent pointwise 95% confidence limits.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal