Abstract
Background: Allogeneic stem cell transplantation (alloSCT) is a potential curative treatment for patients (pts) with myelodysplastic syndrome (MDS), with reported long-term survival of 27% to 54% depending on risk group. Myeloablative conditioning (MAC) considered as standard therapy is associated with substantial treatment related mortality (TRM), especially in older pts or those with therapy related disease (tMDS); on the other hand, high rate of relapse have been reported after reduced intensity conditioning (RIC). Therefore, Polish Adult Leukemia Group (PALG) in cooperation with Polish Pediatric Group for Hematopoietic Stem Cell Transplantation analyzed the outcome of MDS pts transplanted between 2000 and 2013 with respect to conditioning intensity.
Material and methods. Three hundred and four pediatric and adult patients with median age of 38 years (range: 1-69) were retrospectively analyzed. The study cohort included pts with intermediate-2/high risk according to IPSS (136), unfavorable cytogenetics (86), secondary AML (43) and tMDS (35). Among adult pts (216), 74 (34%) were older than 50. The median time between diagnosis and transplant was 8 months (range:1-117). Before transplantation 202 pts had <5% bone marrow blasts, while 48 pts underwent alloSCT with blasts >10%. For conditioning, RIC protocols based on fludarabine were used in 180 pts and 102 pts were treated with myeloablative therapy based on busulphan. Stem cells from related (144) or unrelated (160) donors were grafted in median dose 4.75 (1.3-27.4)x106 of CD34+ cells/kg. Peripheral blood (PB) stem cells were transplanted in 222 pts. Thirty nine pts received allograft from HLA mismatched donors.
Results: Engraftment occurred in 285 (94%) pts and 8 pts died before +21 day after transplantation. Infectious complications were observed in 252 (82%) pts during neutropenia (febrile of unknown origin 163, bacterial 53, fungal 24, bacterial and fungal 12). Late infections, assessed in those who survived 100 days, occurred in 130 (50%) pts, and were related mainly to CMV infection. Severe toxic complications (CTCAE grade 3-4) developed in 67 (22%) pts. Acute graft versus host disease (GVHD) grade 2-4 occurred in 77 (27%) pts, while chronic extensive GVHD in 37 (14.5%) pts. Forty seven pts experienced disease relapse after treatment.
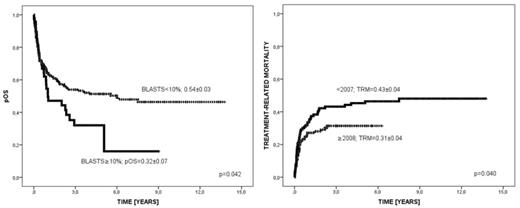
Over a median follow-up of 43 months (range: 15-70) 156 (51%) pts were alive. In 44 cases deaths were related to relapse, 36 pts died due to GVHD, 43 due to infection and 25 because of organ toxicity. Probability of 3-years overall survival (OS), disease free survival (DFS), relapse incidence (RI) and TRM were 0.51±0.03, 0.50±0.03, 0.18±0.03 and 0.47±0.03, respectively. OS (0.56±0.04 vs 0.44±0.04, p=0.036) and TRM (0.31±0.04 vs 0.43±0.04, p=0.040) were statistically better for pts transplanted after 2007 (Figure 1).
In multivariate analysis the only factors associated with lower OS were bone marrow blasts before alloSCT >10% (p=0.05, HR 1.5), mismatched donor (p=0.015, HR 1.8), PB as source of stem cells (p=0.048, HR 1.5) and alloSCT performed after 2007 (p=0.029, HR 1.6). There were no statistically significant differences in OS, DFS, RI and TRM between pts conditioned with RIC or MAC when analyzed in whole study cohort or with respect to age group, IPSS risk group, cytogenetics, interval from diagnosis to alloSCT.
Conclusions: Allogeneic SCT is an option for MDS patients in different age groups. Disease status at time of transplant, mismatched donor and PB source of stem cells, but not conditioning intensity are the most important determinant for the outcome. High rate of TRM remains a concern, despite improvement over time.
Results of alloSCT in MDS
Jedrzejczak:Amgen, Novartis : Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal