Abstract
Title: Serum Uric Acid Levels during Allogeneic Hematopoeitic Cell Transplantation and Subsequent Graft Versus Host Disease
Acute graft-versus-host disease (aGVHD) is a donor T-cell driven response against host tissue that can complicate allogeneic hematopoietic cell transplantation (HCT). The initiation of aGVHD is thought to involve the stimulation of antigen presenting cells through exposure of the immune system to endogenous "danger signals" from dying cells, which can result from the cytotoxic effects of conditioning regimens. The identification of uric acid as one such critical factor released from injured cells was discovered over the past decade, and subsequent animal studies have demonstrated that suppressing uric acid can reduce T-cell activation. Furthermore, a phase I study of patients undergoing myeloablative allogeneic HCT at our institution suggested that the use of urate oxidase may modulate the development of aGHVD, presumably through lowering uric acid levels.
In this retrospective study, we tested the hypothesis that patients who developed aGVHD have increased peri-transplant uric acid levels compared to those who did not. We included those who underwent myeloablative allogeneic HCT from 2007 to 2011 who were not enrolled in the aforementioned phase I study. Sixty-six patients with hematologic malignancies (AML=35, MDS=11, NHL=10 ALL=6, MPD=2, MM=1, CML=1) were analyzed. Notable transplant characteristics include conditioning regimen (Bu/Cy=26, Bu/Flu=29, Cy/TBI=7, Bu/Clo=3, Clo/TLI=1); donor status: matched related donor (MRD=40), matched unrelated donor (MUD=26); disease status: complete remission (CR=39), relapsed/refractory (R/R=27), and type of GVHD prophylaxis: cyclosporine based (CsA/MTX=24, CsA/MMF=3), tacrolimus based (Tac/MTX=16, Tac/MTX/ATG=17, Tac/MTX/Sirolimus=6). Serum uric acid levels were collected from day -7 to day +10 of transplant (up to 18 days recorded per patient). All patients received allopurinol from day -7 to day -1 per institutional protocol.
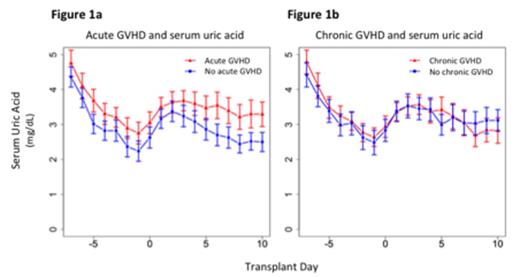
On average, daily serum uric acid levels were recorded in 15.6 out of the 18 days designated per patient, and 83% (N=55) of patients had levels measured up to day +10 of transplantation. The incidence of aGVHD of any grade was 64% (N=42) and 45% (N=30) for grades II-IV. The incidence of mild or limited cGVHD was 35% (N=23) and moderate/severe or extensive cGVHD was 17% (N=11). Those who developed aGVHD had a significantly higher level of serum uric acid compared to those who did not: pre-transplant (d-7 to d0) period (p=0.003), post-transplant (d1 to d10) period (p<0.001) [Figure 1a]. Those who developed cGVHD had no statistically significant difference in serum uric acid levels compared to those who did not: pre-transplant (p=0.22), post-transplant (p=0.69) [Figure 1b]. Subgroup analyses showed that patients with R/R disease with aGVHD had significantly higher uric acid levels than those without aGVHD: pre-transplant (p<0.001); post-transplant (p<0.001), while patients in CR had similar uric acid levels: pre-transplant (p=0.48); post-transplant (p=0.45). Patients treated with cyclosporine or tacrolimus based prophylactic regimen showed similar trends in uric acid levels between aGVHD groups in the post-transplant period.
These results suggest that elevated uric acid levels peri-transplantation may be associated with increased incidence of aGHVD but not cGVHD and may be more relevant in patients with more advanced disease. As a cause-effect relationship of uric acid levels and GVHD cannot be ascertained based on this retrospective data, future prospective studies will be required to clarify this association.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal