Abstract

<Introduction>
Early central nervous system (CNS) complications have been associated with significant morbidity and mortality after allogeneic stem cell transplantation (Allo-SCT). However, the incidence, etiology and clinical characteristics of early CNS complications have not been well understood. Moreover, the impact of stem cell sources on early CNS complications remains to be determined.
<Methods>
To address these issues, we retrospectively reviewed the medical record of 723 consecutive patients who underwent first Allo-SCT at Toranomon Hospital between 2006 and 2013. Early CNS complications were defined as distinct CNS manifestations such as convulsion, change of mental state, defect of short-term memory, or focal motor or sensory symptoms, occurring within 100 days post-transplant. The etiology of CNS complications was determined by clinical, radiologic, or microbiological finding or a combination of these factors. Patients who developed transient consciousness disturbances in septic state or circulatory collapse, had a history of brain surgery, or showed change of mental status at the terminal stage of multiple organ failures, were excluded from CNS complications. CNS relapses of underlying diseases were also excluded from this analysis.
<Results>
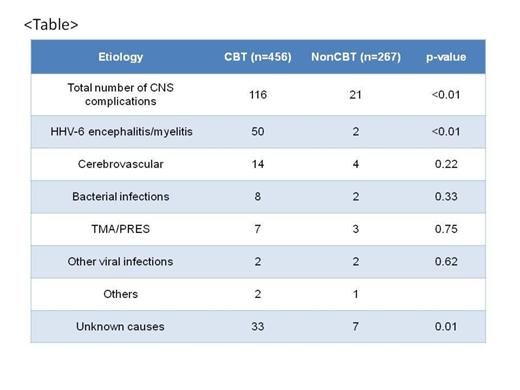
Their median age was 56 years (range, 16-82). Underlying diseases were AML in 360, MDS/MPD in 76, CML in 21, ALL in 82, ATL in 30, HL in 11, NHL in 109, AA in 23 and others in 11. Four hundred ninety-nine (69%) were not in remission at the time of transplant. Three hundred ninety-five patients (54.6%) were conditioned with myeloablative regimens, whereas 328 patients received reduced-intensity regimens. Donor sources consisted of related peripheral blood /bone marrow (BM) (n=101), unrelated BM (166) or cord blood (456). One hundred thirty-seven developed CNS complications on median of 25 (3-89) days post-transplant. Cumulative incidence of CNS complications at 100 days was 19%. The etiology included human herpesvirus 6 (HHV-6) encephalitis/myelitis (n=52), Non HHV-6 viral infections (4), bacterial infections (10), cerebrovascular diseases (18), thrombotic microangiopathy (TMA) / posterior reversible encephalopathy syndrome (PRES) (10), others (3) and unknown causes (40). With median observation period of survivors of 791 (27-2919) days, overall survival at 2 years was 26% in patients who developed CNS complication and was significantly worse than in those who did not develop it (46%, p<0.01) (Figure). In univariate analysis, disease status (high risk or standard risk), recipient age (age<55 or ≥55), underlying disease (lymphoid or others) had no impact on the incidence of early CNS complications. Patients who received cord blood transplantation (CBT) showed significantly higher incidence of CNS complications compared to those receiving other donor sources (25.5% vs 7.9%, p<0.01). In multivariate analysis, CBT was the only significant risk factor for CNS complications (HR=3.59, 95% CI 2.26-5.70, p<0.01). Incidence of HHV-6 encephalitis/myelitis was significantly higher in CBT recipients than other donor sources (11.0% vs 0.7%, p<0.01) (Table). Interestingly, the incidences of infectious complications other than HHV-6 were comparable between donor sources, suggesting there is a preferential vulnerability to HHV-6 infections in CB recipients. We have recently reported close association between the development of pre-engraftment immune reactions (allo-immune reactions unique to CBT) and of HHV-6 encephalitis (ASH 2012). Not just slow immune reconstitution following CBT, but other immune-mediated mechanisms may have contributed to the development of HHV-6 encephalitis.
<Conclusion>
Early CNS complications are serious concerns leading to inferior survival rate after Allo-SCT. Cord blood recipients are at higher risk for developing CNS complications, particularly of HHV-6 associated. Mechanisms behind them and optimal treatment approaches need to be clarified further to improve outcome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal