Abstract
Background: Chronic myelomonocytic leukemia (CMML) is an uncommon and heterogeneous disease with a varying clinical course. Treatment with hypomethylating agents is associated with a low incidence of complete remission and an ongoing risk of transformation to acute leukemia. Treatment strategies for CMML are expanding however allogeneic stem cell transplant (alloSCT) remains the only curative therapy. Transplant outcome data for CMML are limited and often pooled with other myelodysplastic syndromes. This retrospective study aimed at studying the transplant outcomes and identifying prognostic factors for survival and relapse in 57 patients with CMML transplanted in Australia between Jan 2000 and Dec 2013.
Methods: A retrospective review of CMML patients transplanted in Australia was undertaken. Data analysed included recipient demographics, donor/graft characteristics, and conditioning details. Additional patient data at transplant for published prognostic factors (unfavorable factors included hemoglobin (Hb) < 120g/L, transfusion dependence, leucocyte count > 13 x 109/L, absolute lymphocyte count greater than 2.5 x 109/L, circulating immature myeloid cells, bone marrow blasts 10% or more, karyotype) were analyzed (Onida et al, Blood 2002, 99:840, Such et al, Haematologica 2011,96:375). Overall survival (OS) and progression free survival (PFS) were calculated using the Kaplan-Meier estimate with intergroup comparison with logrank test and multivariate analysis using Cox proportional hazards modelling. Cumulative incidences of non-relapse mortality (NRM), relapse and acute and chronic graft-versus-host disease (GVHD) were calculated accounting for competing risks using the method of Fine and Gray with intergroup comparison and multivariate analysis using competing risk regression.
Results: 57 patients with CMML underwent 60 alloSCT between Jan 2000 and Dec 2013. Patient characteristics were as follows: M/F 41/16, Median age was 56 years (y) (range15-68 years). 12(21%) had palpable splenomegaly, 11(19%) leucocyte count > 13 x 109/L, 23 (40%) had circulating immature myeloid cells and 10(18%) had a lymphocyte count greater than 2.5 x 109/L. 29(50%) of the patients had transformation to acute leukemia prior to transplant. 31/14/7/5 had good/ intermediate/high/unknown cytogenetic. 22(38%) were untreated prior to transplant, while 30 (52%) received intensive chemotherapy and 2 (3.5%) received hypomethylating agents pre transplant.
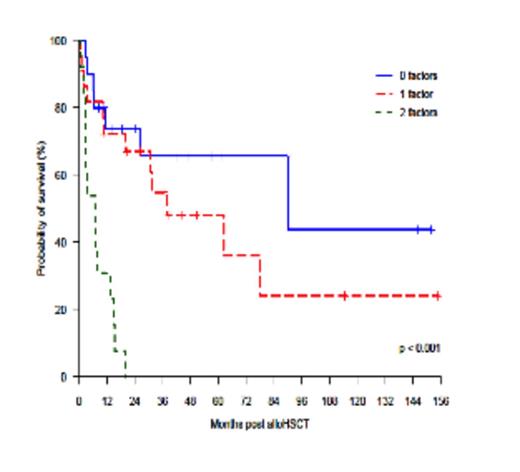
33 (55%) were matched related donor transplants. The graft source used was peripheral blood stem cells in 54(90%) transplants. Myeloablative conditioning was used in 28 (47%) transplants. Median follow up of all patients was 15.3 months (0.6-154.9 months). Median follow up of the survivors was 40.1 months (7.5-154.9 months). OS and PFS at 6 years was 40% (95% CI 27- 58 %) and 27% (95% CI 15-46 %) respectively. NRM and incidence of relapse at 6 years were 39% (95% CI 23-54%) and 35% (95% CI 20-50%) respectively. Cumulative incidence of aGVHD grade 2-4 at day 100 was 39% (95% CI 26-52%) and grade 3-4 at day 100 was 25% (95% CI 13-36%). Cumulative incidence of any cGVHD and extensive cGVHD at 1 year was 40% (95%CI 26-54%) and 26% (95% CI 14-39%) respectively. There was no impact of transplant year, prior leukemic transformation, transfusion dependence, leucocyte count, cytogenetic and splenomegaly pre transplant, conditioning intensity and donor gender mismatch on survival outcomes post transplant. In multivariate analysis, age < 50y, non-sibling donor and lymphocyte count greater than 2.5 x 109/L were adverse risk factors for OS and PFS. The adverse outcome in young patients may be an outcome of disease biology. A survival model based on the presence of 0,1 or 2 factors revealed a 6 year OS of 66% (95%CI 46-94), 36% (95% CI 17-76%) and 0% respectively (Fig1). Bone marrow blasts pre transplant (10% or more) were independently associated with a higher risk of relapse post transplant.
Conclusion: AlloSCT is a curative treatment for CMML but the high NRM and relapse rates continue to remain significant issues. A high lymphocyte count pre transplant was noted to influence survival post transplant. Influence of pre transplant bone marrow blasts on relapse risk indicates importance of disease state pre transplant. Outcomes of alloSCT in CMML remain superior to current existing therapies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal