Abstract

Introduction: Invasive aspergillosis (IA) frequently occurs during treatment for acute leukemia. Historically IA has been a major barrier for allogeneic hematopoietic stem cell transplantation (allo-HSCT). In the recent decade there has been significant improvement of anti-fungal management including novel anti-fungal agents and diagnostics. The influence of invasive IA on long term survival and on transplant related complications has not been investigated in a larger patient cohort under current conditions.
Specific Aim: The aim of this retrospective study was to analyze the long term outcome of patients undergoing allo-HSCT with history of prior proven, probable and possible IA as compared to patients without history of IA.
Methodology: Patient-, disease-, and transplant-related variables were collected according to the data entries in the EBMT database. Inclusion criteria were as follows: first allo-HSCT performed between 2005 and 2010 in patients with acute leukemia; availability of data on IA prior to allo-HSCT. The median time of death after allo-HSCT was estimated using the Kaplan-Meier method and cohorts were compared by the log-rank test. The following variables entered the multivariate model as possible confounders: age (as continuous variable), gender (M vs. F), underlying disease (ALL vs. AML), status at SCT (1st CR vs. ≥2 CR vs. Prim Refr/noCR), time from diagnosis to SCT (as continuous variable), donor type (sibling vs. matched UD vs. mismatched UD vs. Haplo), source of SCT (BM vs. PB vs. CB), donor age, d/r gender match, d/r CMV status, conditioning regimens (MAC vs. RIC, TBI yes/no), type of immunosuppression (in vivo T depletion y/n, in vitro T-depletion y/n). The cumulative incidences were computed using the cumulative incidence method. Differences between the two cohorts were verified with the Gray test.
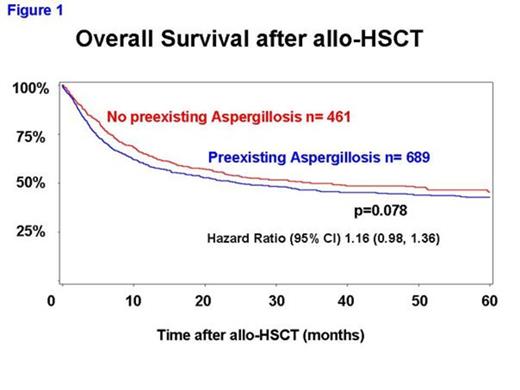
Results: 1150 patients fulfilled the entry criteria and were included in the analysis (patient characteristics, table 1). The median follow up time was 52.1 months (95% CI 49.0, 56.6). The impact of prior IA on overall survival in allo-HSCT recipients with acute leukemia was not statistically significant (figure 1). We detected no significant differences in the cumulative incidence of acute GVHD grade II-IV [29.1% IA vs. 32.0% no IA, p=0.27, hazard ratio (HR) (95% CI) 0.89 (0.71, 1.10)]; chronic GVHD [43.9% IA vs. 49.3% no IA, p=0.26, HR (95% CI) 0.89 (0.73, 1.09)]; relapse [33.7% IA vs. 33.0% no IA, p=0.35, HR (95% CI) 1.11 (0.9, 1.36)] and pulmonary complications [8.3% IA vs. 6.9% no IA, p=0.4, odds ratio (95% CI) 1.21 (0.77, 1.90)]
Conclusion: Prior IA had no significant impact on transplant-related complications and overall survival in this large data set of patients with acute leukemia undergoing allo-HSCT. We speculate that an overall better management of IA may have contributed to this result. Considering that we did not assess the impact of the type of IA (proven/probable vs. possible) and the status of IA before allo-HSCT, these data deserve to be confirmed by a prospective study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal