Abstract
Background: Immune thrombocytopenia (ITP) in adults is generally a chronic disorder that may lead to severe thrombocytopenia and bleeding. Though several medical modalities such as thrombopoietin receptor agonists have become available for the management of ITP withinin the last decade, splenectomy remains a valuable option for management of refractory ITP, with approximately 2/3 of treated patients remaining in complete remission 10 years afterwards. However, there are no consistent and reliable predictors of splenectomy response for an individual patient with ITP. Since patients with ITP who fail to respond to splenectomy can develop significant bleeding in the postoperative period it is important to identify those individuals early after their surgical procedure so that aggressive medical intervention may be employed. Despite this concern, there is little information available on the value of postoperative platelet counts obtained soon after splenectomy in predicting the ultimate outcome of surgery.
Objectives: The goal of this study was to define the value of platelet counts determined soon after splenectomy on the ultimate success of splenectomy in inducing remission of ITP.
Methods: We reviewed the medical records of 66 patients who underwent splenectomy for ITP at the Cleveland Clinic from 2000-2013. A complete response was defined as a stable platelet count >100 x109/L two months after splenectomy without medical therapy. Stepwise logistic regression with backward selection was used to identify significant predictors of complete response.
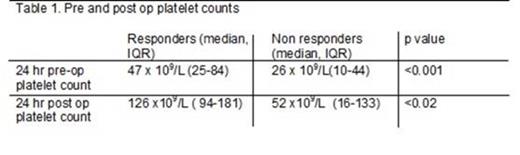
Results: The 66 patients had a median age of 41(IQR 21-56) with a male:female ratio of 1:2. The median platelet count at the time of diagnosis was 12 x 109/L and 43% of the patients had severe ITP (defined per IWG guidelines as bleeding that mandates treatment). Ninety percent of patients were steroid dependent, and 39%, 15% and 5% had been treated with rituximab, eltrombopag or romiplostim respectively. The median time to splenectomy from diagnosis of ITP was 22 months (IQR 6-44 months). At a median follow up of 35 months after splenectomy, 39 patients (59%) achieved a complete response. The median platelet count prior to and 24 hours after splenectomy in responders and non-responders is shown in Table 1.
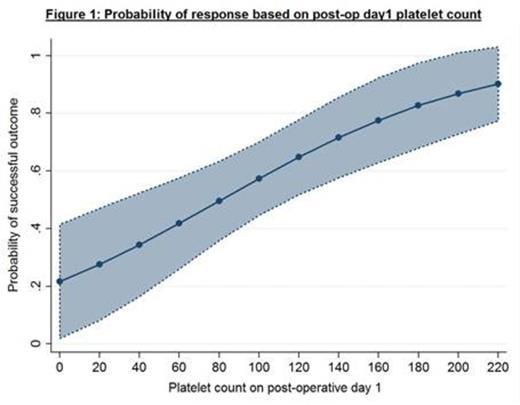
Logistic regression analyses identified a post-op day 1 platelet count greater than the median platelet count of 112 x 109/L (OR- 3.72, CI- 1.14-12.16, p<0.03) and post-operative day 3 platelet count greater than median platelet count of 175x 109/L (OR- 4.87, CI- 1.37-17.2, p<0.01) as a significant predictor of splenectomy response. The probability of response based on the post-operative day 1 platelet count is depicted in Figure 1. The difference between the pre-splenectomy and post-operative day 1 platelet count was also a significant predictor of response (OR 1.01 (1.0001-1.02), p=0.04), (figure 2). The log of the time from the diagnosis of ITP to splenectomy (OR- 0.61, CI 0.40-0.94, p<0.02) was also a weak, but significant predictor. Increased numbers of prior treatments for ITP prior to splenectomy correlated with a decreased response, although this relationship was not statistically significant.
Conclusion: The platelet count on postoperative day 1 is a significant predictor of long term response to splenectomy, with almost 4-fold increased probability of achieving remission if this value is >112 x 109/L .This is among the first studies to examine the prognostic value of the platelet count obtained this early after splenectomy, and suggests that in patients with severe ITP and a persistently low postoperative platelet count on day 1, medical therapy should be considered to prevent bleeding. Our data also suggests that responses to splenectomy may be less frequent in patients with a longer interval between ITP diagnosis and splenectomy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal