Abstract
Background: Vascular injury causes platelets to initiate hemostasis by first adhering to exposed subendothelial matrix proteins such as collagen. While the biochemical and biological aspects of platelet adhesion via collagen and von willebrand factor are well characterized, if and whether the mechanical properties of the subendothelial matrix affect platelet function is relatively unknown. As purely mechanical cues, such as substrate stiffness, from collagen matrices are sensed and transduced by endothelial cells to alter their physiological processes, platelets may also exhibit similar behavior (Chein S., AM J Physiol Heart Circ Physiol, 2007). In addition, recent reports demonstrate that the stiffness of the subendothelium varies in different disease states, including atherosclerosis and changes associated with aging (Stroka KM & Aranda-Espinoza H, Blood, 2011). Therefore, understanding the effect of subendothelium stiffness on platelet adhesion, spreading, and activation will provide insight into how biomechanical and biochemical factors interact during clot formation in health and disease. To that end, we fabricated polyacrylamide (PA) gels of varying stiffnesses covalently conjugated with collagen to model the biomechanical properties of the subendothelium. Via differential crosslinking, the stiffness of these PA gels can be varied while maintaining constant collagen concentrations on the gel surface, enabling decoupling of mechanical and biochemical cues (Lam, et al, Mol Cancer, 2010; Pathak A & Kumar S, P Natl Acad Sci, 2012). With these systems, we investigated how the stiffness of the underlying collagen matrix affects platelet adhesion, spreading and activation under static and flow conditions and used pharmacological cytoskeletal inhibitors to investigate the underlying mechanotransductive mechanisms.
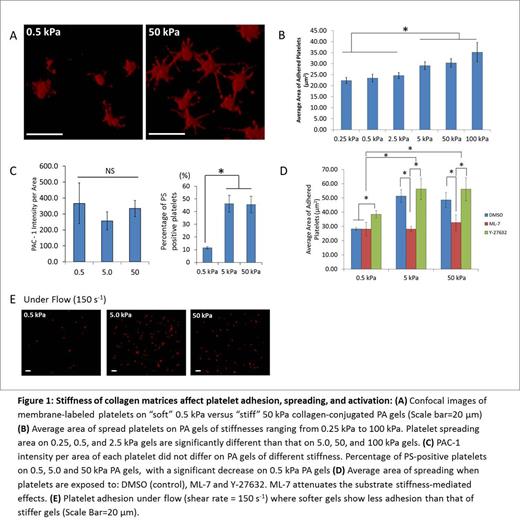
Results and Discussions: Type I collagen was covalently conjugated to the surface of PA gels with varying substrate stiffnesses (0.25 to 100 kilopascals (kPa)); the range of vessel wall stiffness in vivo. The PA gels were then incubated with 5.5 x 106 platelets/ml for 1 hour and stained with a fluorescent membrane dye. While collagen substrate stiffness did not affect platelet adhesion, determined by the number of platelets on each gel, significant differences were observed in platelet spreading area on collagen-conjugated PA gels with stiffnesses >2.5 kPa compared to PA gels of <2.5 kPa (Fig. 1A and 1B). Using PAC-1-FITC and Annexin-V-AF488 to measure platelet integrin αIIbβ3 activation and platelet phosphatidylserine (PS) exposure, respectively, we found that varying the substrate stiffness of collagen matrices did not affect αIIbβ3 activation on adherent platelets but did result in differential levels of PS exposure on adherent platelets, with increased PS exposure on stiffer PA gels (Fig. 1C). In addition, using the myosin light chain kinase (MLCK) inhibitor ML-7 and the Rho kinase inhibitor Y-27632, we observed that platelet exposure to ML-7 eliminated the substrate stiffness-mediated effect on platelet spreading as platelet spreading on PA gels stiffer than 5 kPa was decreased to the levels of that on soft PA gels of 0.5 kPa. Y-27632 exposure did not cause a similar effect, as platelet spreading was increased for all stiffness conditions (Fig. 1D). Finally, under flow conditions using a shear rate of 150 s-1, platelet adhesion in addition to platelet spreading was mediated by substrate stiffness (Fig. 1E); possibly due to weaker collagen attachment on softer substrates that cannot sufficiently resist drag forces.
Conclusion: Our results indicate that platelets adhered on collagen mechanosense the stiffness of the underlying subendothelial substrate and transduce these cues into differential levels of adhesion, spreading and activation. While MLCK mediates aspects of this process, further mechanistic studies are currently being conducted. In addition, as shear stress might interact with the observed substrate stiffness-mediated phenomenon, additional experiments under flow at different shear rates are also ongoing.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal