Abstract
Background: Vitamin D deficiency (VDD) is highly prevalent among patients with sickle cell disease (SCD). Although little is known about the risk factors for VDD in SCD, it has been shown that VDD is associated with chronic pain, bone fragility, and pulmonary function in SCD. In this study we investigated the potential clinical predictors for VDD in patients with SCD.
Method: In a retrospective, cross-sectional analysis, a total of 167 adults with SCD treated at the University of Illinois Medical Center with a baseline 25-hydroxy vitamin D (25-OHD) measurement were screened. Clinical variables were recorded from a clinic visit at least four weeks from a vaso-occlusive pain episode or red blood cell transfusion. Statistical association between 25-OHD and other clinical parameters were investigated.
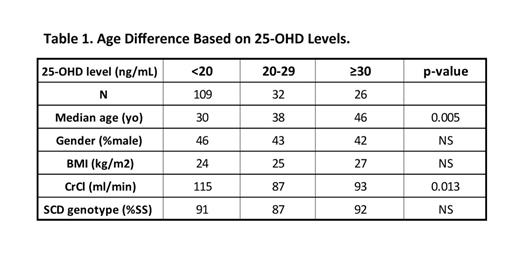
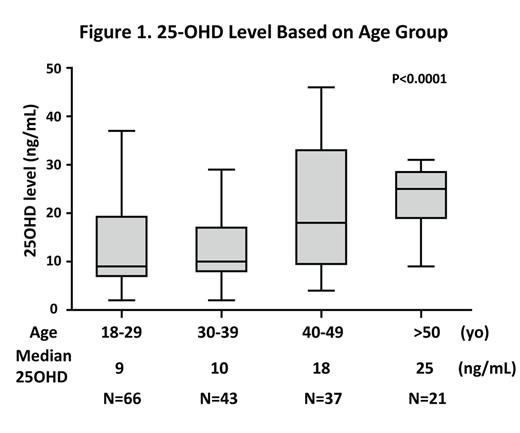
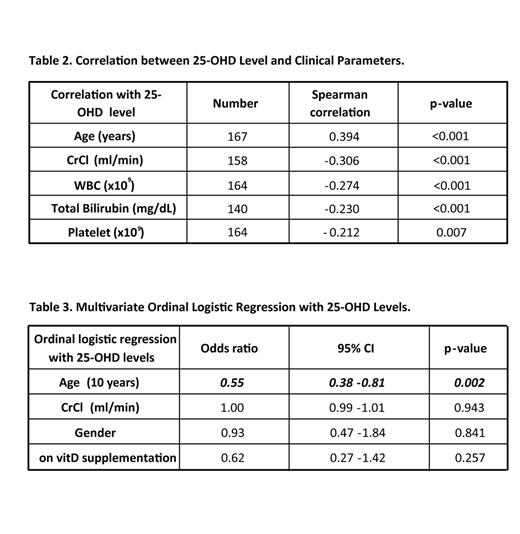
Results: After stratifying the patients based on 25-OHD levels, we observed the median age was significantly younger in patients with lower 25-OHD levels (Table 1). When analyzing different age groups by Kruskal Wallis analysis, 25-OHD levels were significantly elevated in patients ≥ 40 years old (Figure 1). When using Spearman correlation analysis, the 25-OHD levels as a continuous variable positively correlated with increasing age (p<0.001); they also showed a significant negative relationships with creatinine clearance, total bilirubin, platelet count, and white blood cell count (Table 2). Using ordinal logistic regression, age was an independent predictor of 25-OHD levels, as a three-categorical variable, in SCD (OR 0.55, 95% CI: 0.38 – 0.81; p =0.002) after adjusting for gender, creatinine clearance, and vitamin D supplementation (Table 3), which means that younger patients has higher chance of VDD. In the patients with VDD (25-OHD <20 ng/mL), weekly supplementation with oral ergocalciferol (50,000 units for twelve weeks) substantially improved 25-OHD levels (9.9 vs 23.7 ng/mL, p<0.0001, N=24). During a median of 40-month follow-up (range 0 to 96 months), thirteen patients died, but the log rank test or multivariate Cox regression analysis failed to show statistical significance between 25-OHD levels and mortality after adjusting ESRD and baseline vitamin D supplementation, likely due to a short follow-up period and a small sample size.
Summary: Lower 25-OHD levels were associated with younger age in patients with SCD, especially patients younger than 40 years old. One possible explanation is that lower 25-OHD levels may be linked to higher mortality in SCD, but future research is needed to clarify the association between VDD and mortality in SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal