Abstract
Positron emission tomography (PET) is increasingly employed both to guide response-adjusted therapeutic strategies and to provide prognostic information in patients with Hodgkin Lymphoma (HL). The presence of residual [18-F]FDG-avid lesions prior to autologous stem cell transplantation (ASCT) confers a poor prognosis in terms of relapse risk and event-free survival outcomes, even when analysis is restricted to those with chemo-sensitive disease. The prognostic power of PET in the setting of allogeneic SCT remains more contentious, with relatively little data currently published. Information is particularly sparse in terms of outcomes relating to specific histological subtypes of lymphoma.
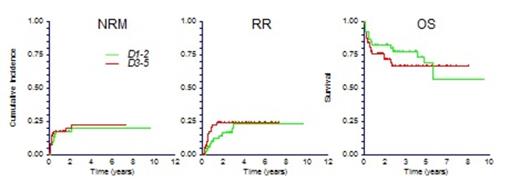
We identified 160 patients transplanted for HL at four UK transplant centers using T-cell depleted conditioning regimens, based either on fludarabine-melphalan-alemtuzumab (FM-C) or the BCNU-etoposide-cytarabine-melphalan-alemtuzumab (BEAM-C) backbone, in whom pre-transplantation PET data were available. These represent the primary data set. Median age was 30 (12-66) years; 59 had failed a prior ASCT and these patients more commonly received FM-C (56/59 vs 26/101, p<0.001); median number of prior lines of treatment was 4 (2-10); median follow-up was 3.1 years in patients remaining alive. A Deauville score could be assigned according to a visual analysis 5-point scale in 137 cases following central review of digital file data; D1-2 (metabolic complete response) n=54, D3 n=13, D4 n=36, D5 n=34. Of those with a D5 score, 18 were non-progressive, and 16 progressive (D5p) prior to transplant. Overall survival (OS) was significantly worse in the D5p subset (19% [0-41%] at 4 years, p=0.001); it did not differ significantly between D1-2 vs D3-5 (78%[66-90%] vs 67%[54-80%], p=0.626), although the OS curves demonstrated early divergence from years 1-4 followed by convergence at later time points (Figure). The worse OS in the D5p cohort related both to a higher non-relapse-related mortality (NRM)(29%[12-65%] at 1 year) and a higher relapse risk (RR)(38%[19-76%] at 4 years). The latter were equivalent for the D1-2 vs D3-5 cohorts (NRM 17%[9-31%] vs 17% [10-30%] at 1 year; RR 23%[13-40%] vs 24% [15-38%] at 4 years respectively)(Figure). Interestingly the kinetics of relapse differed between the latter 2 groups, with relapse occurring later in the D1-2 cohort, again illustrated by early divergence (RR 16%[9-31%] vs 24%[15-38%] at 2 years) followed by later convergence from year 4. Progression free survival was also equivalent (57%[43-72%] vs 54%[41-67%] at 4 years respectively, p=0.347). Although the number of patients with non-progressive D5 scores was relatively small, exploratory analyses revealed no significant differences in survival outcomes between those with D4 vs D5 scores. Analysis of survival outcomes of D1-3 vs D4-5 also revealed no statistically significant differences.
In summary, these data from a large cohort of patients with HL undergoing T-cell depleted allogeneic SCT illustrate inferior outcomes in those with progressive disease prior to transplantation, an altered kinetic of relapse and early survival advantage for those with Deauville 1-2 PET scores compared to those with non-progressive Deauville 3-5 PET scores, but no statistically significant differences in longer term outcomes including relapse risk, PFS and OS. Importantly, these data suggest that the allogeneic graft-versus-tumor activity likely overcomes the poor prognostic impact that has been demonstrated with residual metabolically active disease in the context of conventional dose escalation and ASCT, supporting further exploration of response-adjusted transplantation algorithms.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal