Abstract
Background
Recent studies have shown that mutations in internal tandem duplication (ITD) of the FLT3 gene (FLT3-ITD) influence prognosis of cytogenetically normal AML. Our previous decision analysis (Kurosawa et al, Blood 2011) showed that, for patients with cytogenetically standard-risk AML in first complete remission (CR1), allogeneic hematopoietic cell transplantation (HCT) provided better survival with and without a quality-of-life (QOL) adjustment. In this study, we undertook a decision analysis to determine a favored treatment strategy for patients with cytogenetically standard-risk AML in CR1 depending on FLT3-ITD profile.
Patients and Methods
Inclusion criteria comprised patients aged 16 to 70 years who were diagnosed with intermediate- or unknown-risk AML according to the Southwest Oncology Group cytogenetic classification, and achieved CR1. We collected bone marrow or peripheral blood samples obtained at diagnosis for patients registered, and retrospectively analyzed mutations of FLT3-ITD using DNA extracted from the specimens. We constructed a Markov decision model to reflect outcomes of HCT and chemotherapy in CR1 with three Markov health states; (1) alive after HCT, (2) alive after chemotherapy, or (3) dead. After the decision node of HCT, we added a branch to consider patients who had relapse before receiving HCT in CR1. Cycle length was 3 months and the analyses were performed for 40 cycles, 10 years. Transition probabilities between health states were calculated from the underlying survival rate of the cohort registered. Results were obtained as life expectancy (LE) and QOL-adjusted life expectancy (QALE). We conducted another cross-sectional study to investigate patient-reported QOL from those treated for acute leukemia. Adjusted means of EQ-5D index were adapted from the study as utility estimates that reflect QOL after HCT or chemotherapy (overall mean: post HCT overall, 0.74; post HCT with GVHD, 0.67; post chemotherapy overall, 0.70), and were allowed to change over time (<1 years, 1-2 years, 2-5 years, and 6 years or later from CR1). The analyses were performed using TreeAge Pro software package (TreeAge Software, Williamstown, MA), Stata version 13 (Stata Corp., College Station, TX), and SPSS software (SPSS Inc).
Results
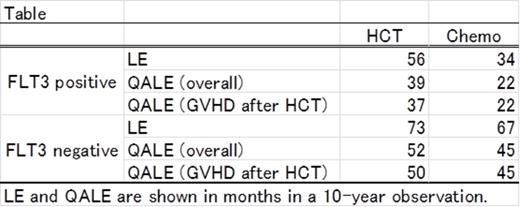
Among 541 patients registered in the database, mutations in FLT3-ITD were successfully tested in 332 patients (61%). The median age of patients was 52 years and the median follow up was 37 months among survivors. FLT3-ITD mutations were found in 60 patients (18%). Eighty-five patients received allogeneic HCT in CR1 and the other 247 patients were treated with chemotherapy alone during the period of CR1. Patients who received HCT were significantly younger (median age, 41 vs 54 years), more frequently received 2 courses of induction therapy and had dysplasia at diagnosis compared to those who were treated with chemotherapy. In FLT3-positive and FLT3-negative patients, similar proportions of patients received HCT in CR1 (23%, N=14 vs 26%, N=71). In 10-year observation, LE and QALE were 5.9 and 5.1 years, respectively, for total patients. For FLT3-positive patients, allogeneic HCT in CR1 improved LE and QALE by 22 and 17 months, respectively (Table). QALE benefit of HCT was still apparent when we used utility estimates for post HCT with GVHD. Sensitivity analyses across the range of plausible utility estimates (HCT, 0.63-0.83; chemotherapy, 0.64-0.75) did not change the conclusion. For FLT-3 negative patients, HCT benefit was less than 1 year for LE and QALE. Sensitivity analyses showed that chemotherapy would be the preferred strategy when utility estimates for chemotherapy was higher than 0.7. An analysis of FLT3-negative patients stratified by age indicated that HCT in CR1 provided better LE and QALE than chemotherapy alone for patients aged 55 years or older (LE: 77 vs 57; QALE: 54 vs 38 months). In contrast, HCT did not improve LE (74 vs 79 months) or QALE (52 vs 54 months) compared to chemotherapy alone in younger patients with FLT3-negative AML.
Conclusion
For patients with FLT3-ITD-positive, cytogenetically standard-risk AML, allogeneic HCT in CR1 offered overall and QOL-adjusted survival benefit. For patients without FLT3-ITD, survival benefit of HCT in CR1 was less apparent.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal