Abstract
Background: The role of autologous stem cell transplantation (ASCT) in follicular lymphoma (FL) in the rituximab era remains undefined. Although ASCT has demonstrated to improve outcomes in relapsed/refractory (R/R) FL, there are very few studies addressing this issue in patients who had prior exposure to rituximab. Our aim was thus to assess the outcome of ASCT in FL patients in the modern era.
Methods and Patients: We conducted a single center retrospective analysis of patients who underwent ASCT for follicular lymphoma at the Cleveland Clinic. Patient and disease characteristics were examined and prognostic factors for survival were determined using univariate and multivariate Cox analysis.
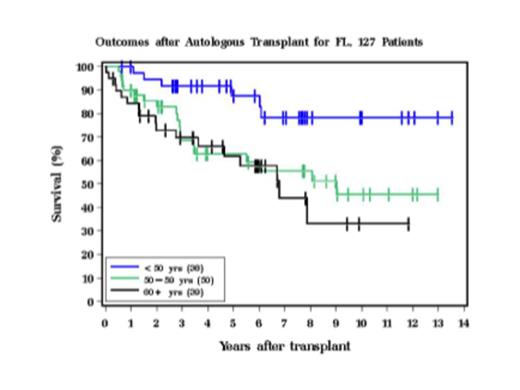
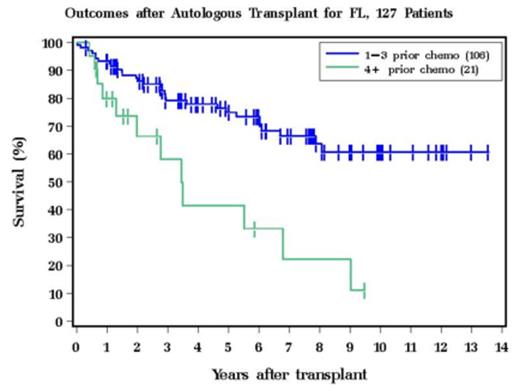
Results: Total of 127 patients with a confirmed diagnosis of FL underwent ASCT at our institution between March 2000 and October 2013. Study population was predominantly male (61%) and Caucasian (92%). Median age at transplant was 55 years. Majority of the patients had FL grade of 1-2 (88%), International Prognostic Index (IPI) 0-2 (81%), and stage IV disease (60%) at the time of diagnosis. All, but 9 patients (93%) received rituximab as part of their prior treatment and 53% had received ³3 prior therapies. Disease status prior to transplant was 1st partial response (PR1) (9%), 2nd complete remission (CR2) (24%), 2nd PR (PR2) (60%), and R/R (8%); no patients received transplant in the 1st CR (CR1). An uniform preparative regimen consisting of Busulfan, Cyclophosphamide and Etoposide (Bu/Cy/VP16) was used in all patients. Median CD34+ cell dose was 7.49 x 106/kg. Median days to neutrophil engraftment were 10 days and platelet engraftment was 14 days. In our cohort, 10-year progression free survival (PFS) and overall survival (OS) were 33.2% and 52.4% respectively. Disease relapsed in 58/127 (46%) of the patients and 67% were alive at the time of last follow up. Age at transplant (Figure 1) and number of prior therapies, >3 vs 1-3 (Figure 2) were significant prognostic factors for OS, in both univariate and multivariate analyses. Higher age (HR 1.76, 95% CI 1.23-2.52, p=0.002) and >3 prior therapies (HR 2.58, 95% CI 1.31-5.12, p=0.006) were predictive for inferior OS. Disease status at transplant, IPI, and stage had no impact on survival. Disease relapse (67%) and secondary malignancies (7.1%) were the leading causes of death.
Conclusions: In our analysis, a durable PFS, median of 49 months, was observed in patients with R/R FL who underwent an ASCT in the rituximab era. Age at transplant and number of prior therapies were identified as poor prognostic factors for OS. These data suggest that ASCT should be considered in young patients with R/R FL early in their disease course.
Hill:Millenium: Research Funding; Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal