Abstract
Consolidative autologous stem cell transplantation (ASCT) is a commonly utilized treatment modality for peripheral T cell lymphomas (PTCL) and has been shown to improve progression free survival. The optimal timing of ASCT for PTCL is not well defined and studies have included upfront ASCT or ASCT at the time of relapse. However, long-term outcomes of ASCT, especially when used as upfront consolidation, have not been well described.
Previously published data, including the one from our institution, (Smith S et al BMT. 2007;40:239-243) revealed inferior outcomes following ASCT in relapsed PTCL. We performed a retrospective study to describe our institutional experience in a relatively large cohort of patients with PTCL who were treated with ASCT (N=78) between 1996 and 2013 and had a median follow up of 55 months.
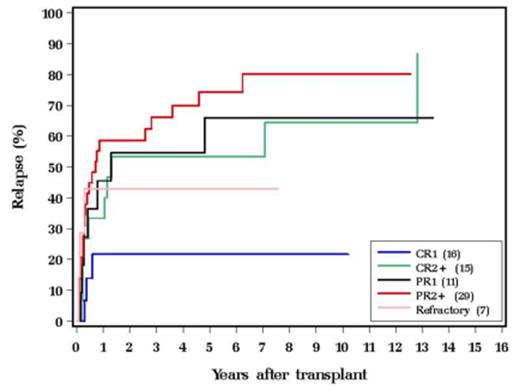
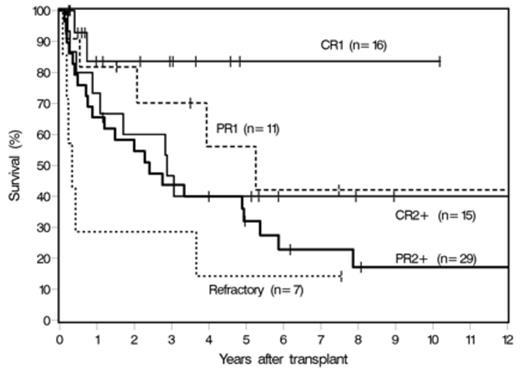
Among these, 62% were male, 89% Caucasian and 84% had a Karnofsky performance score ³90. The subtypes included 26 peripheral T cell lymphomas (PTCL) (33%), 19 anaplastic large cell lymphoma (ALCL) alk- (24%), 13 ALCL alk+ (17%) 16 angioimmunoblastic T cell lymphoma (AITL) (21%) and 4 extranodal NK/T cell nasal type (5%). Prominent disease characteristics at diagnosis included stage III-IV in 80%, and IPI score of 0-3 in 73%. Only 26% had bone marrow (BM) involvement. Majority of the patients (76%) received 2 or more prior therapy. 99% of the transplants was performed using Busulfan, Cyclophosphamide, and Etoposide (Bu/Cy/VP16) preparative regimen. While 27 (35%) patients received ASCT as part of their initial treatment, 51 (65%) patients were transplanted after their disease had relapsed. About one third of our cohort (31%) attained a complete response (CR) post ASCT. The 5-year relapse rate (RR) for CR1, CR2 and PR1 were 22%, 53% and 66% (Figure 1) implying that both the disease status and response prior to transplant are key determinant factors for long-term outcome. The RR curve plateaued after 8 years indicating that a proportion of patients had attained a durable remission. At the time of analysis, 42% were alive. Disease relapse was the cause of death in 76% of the cases. Our 10-year RR, relapse free survival (RFS) and overall survival were 64%, 25% and 31% respectively. On univariate analysis disease status, BM involvement and stage were prognostic for RFS and OS, but only disease status (RFS: HR 2.27, p=0.023; OS: HR 4.75, p=0.006) and BM involvement (RFS: HR 3.10, p=0.019; OS: HR 2.94, p=0.018) retained significance on multivariate analysis. Moreover, disease status was also predictive for relapse in both univariate and multivariate analyses (HR 2.12, 95% CI 1.05-4.27, p=0.035).
Conclusions: In a relatively large cohort of PTCL patients with long-term follow up after ASCT, upfront consolidative autologous stem cell transplantation in chemo sensitive patients resulted in lower RR and improved RFS and OS.
Hill:Millenium: Research Funding; Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal