Abstract
Background: Chronic Graft-versus-host disease (GVHD) has been a serious complication after allogeneic transplantation. The difference of incidences, risk factors and outcomes between unrelated cord blood transplantation (uCBT) and unrelated bone marrow transplantation (uBMT) has not been fully evaluated.
Patients and Methods: We retrospectively analysed the records of 455 adult patients who underwent uCBT or uBMT for the first time at the Toranomon Hospital between 2002 and 2013, and who survived more than 100 days without relapse within 100 days after transplantation. Pre-engraftment immune reaction (PIR) was defined as unexplained fever in the absence of documented infection with skin eruption, peripheral edema and body-weight gain before engraftment. Acute GVHD was graded according to previously described criteria. Chronic GVHD was classified by both traditional criteria and by the 2005 NIH Consensus Criteria. The probability of developing chronic GVHD was estimated on the basis of cumulative incidence curves. Competing events for chronic GVHD were death or relapse without GVHD. The cox proportional hazards model was used to evaluate the effect of confounding variables on chronic GVHD. We also evaluated the effect of chronic GVHD on relapse and overall survival, where the occurrence of chronic GVHD was treated as a time-varying covariate.
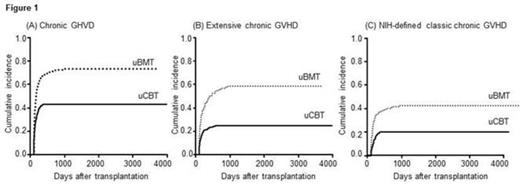
Results: A total of 240 patients were diagnosed with chronic GVHD by traditional criteria at a median onset of 123.5 days after transplantation, with the 2-year cumulative incidence of 54.0%. The incidence was significantly lower after uCBT versus uBMT (43.1% vs. 72.8%, P<0.001, Figure1A). About 70% of the patients (n=163) had extensive type, which occurred less frequently after uCBT versus uBMT (25.0% vs. 56.1%, P<0.001, Figure1B). The most common involved organ was skin (78.8%), followed by liver (36.7%) and gastrointestinal tract (33.3%) in the total population. The uCBT patients showed significantly less frequent involvement of the eye, oral cavity, lung and joint compared to the uBMT patients (all P<0.001), while rates of skin, liver and gastrointestinal tract involvement were not different between the two groups (P=0.64, P=0.18 and P=0.34, respectively). For both the uCBT and the uBMT patients, grade II-IV acute GVHD was identified as the only significant risk factor for traditionally-defined any chronic GVHD (HR 1.48, P=0.03 and HR 1.82, P=0.003) and extensive chronic GVHD (HR 2.51 and HR 2.33, both P<0.001). PIR was identified as a significant risk factor for the extensive chronic GVHD after uCBT (HR 1.69, P=0.04). Of all the 240 patients, 124 patients met the NIH-defined classic chronic GVHD, the 2-year cumulative incidence of which was 28.0%. The incidence was significantly lower after uCBT compared to uBMT (20.1 vs. 41.8%, P<0.001, Figure1C). Thirty-two patients fulfilled the criteria for overlap syndrome. The remaining 84 presented with the NIH-defined persistent (n=31), recurrent (n=40) or late-onset (n=13) acute GVHD, the proportion of which was significantly higher after uCBT versus uBMT (43.1% vs. 26.5%, P=0.02). Both the uCBT and the uBMT patients with NIH-defined classic chronic GVHD had significantly better overall survival (HR 0.10, P=0.001 and HR 0.43, P=0.03), while traditionally-defined chronic GVHD did not significantly improve the survival (HR 0.63, P=0.06 and HR 0.92, P=0.81). Although the uBMT patients with traditionally-defined chronic GVHD and those with NIH-defined chronic GVHD had lower risks of relapse (HR 0.36, P=0.001 and HR 0.49, P=0.05), the influence of the chronic GVHD on relapse was not apparent in the uCBT patients (HR 0.76, P=0.23 and HR 0.60, P=0.15).
Conclusions: The incidence of chronic GVHD was significantly lower after uCBT compared to uBMT. Typical clinical features of chronic GVHD seems to improve overall prognosis in the uCBT patients, although those might not have full effect on reducing the risk of relapse like in the uBMT patients. Prevention of acute GVHD manifestations occurring more than 100 days might further improve the outcome after uCBT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal