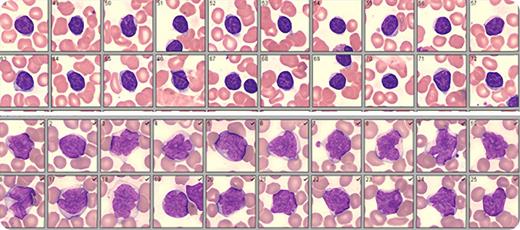
A 77-year-old woman presented with cervical adenopathy. A complete blood count was performed: white blood cells (WBCs), 13.8 × 109/L; absolute lymphocytes, 11.9 × 109/L; hemoglobin, 12.4 g/dL; and platelets, 199 × 109/L. Immunophenotyping of peripheral blood confirmed a diagnosis of chronic lymphocytic leukemia (CLL). Lymphocytes were CD5+, CD19+, CD23+, CD79B+, FMC7−, CD38+, and ZAP70+. Cytogenetics/molecular analysis revealed trisomy 12 and unmutated immunoglobulin heavy chain variable region (IgVH). Positron emission tomography computed tomography showed splenomegaly and widespread adenopathy. WBC differential by digital microscopy (Cellavision) revealed 9% neutrophils, 3% eosinophils, 2% monocytes, 60% lymphocytes, and 26% large abnormal lymphoid cells with clefted nuclei, moderately clumped chromatin, and pale blue cytoplasm. These findings were consistent with French-American-British atypical CLL (aCLL), mixed cell type. Although the possibility of Richter’s transformation could not be ruled out, clinical, laboratory, and radiologic findings did not support this diagnosis (data not shown).
Patients with aCLL may experience more aggressive disease and shortened survival. Also, as was seen in this case, aCLL has been associated with poor prognostic indicators such as unmutated IgVH, CD38+, ZAP70+, and trisomy 12. Digital microscopy is a rapid and inexpensive screening tool that improves the ability to identify aCLL patients. An experienced morphologist can quickly compare/contrast and classify variant lymphocytes as they are presented on a wide-screen monitor. The images are archived for a second review if needed and comparison with previous or subsequent results.
A 77-year-old woman presented with cervical adenopathy. A complete blood count was performed: white blood cells (WBCs), 13.8 × 109/L; absolute lymphocytes, 11.9 × 109/L; hemoglobin, 12.4 g/dL; and platelets, 199 × 109/L. Immunophenotyping of peripheral blood confirmed a diagnosis of chronic lymphocytic leukemia (CLL). Lymphocytes were CD5+, CD19+, CD23+, CD79B+, FMC7−, CD38+, and ZAP70+. Cytogenetics/molecular analysis revealed trisomy 12 and unmutated immunoglobulin heavy chain variable region (IgVH). Positron emission tomography computed tomography showed splenomegaly and widespread adenopathy. WBC differential by digital microscopy (Cellavision) revealed 9% neutrophils, 3% eosinophils, 2% monocytes, 60% lymphocytes, and 26% large abnormal lymphoid cells with clefted nuclei, moderately clumped chromatin, and pale blue cytoplasm. These findings were consistent with French-American-British atypical CLL (aCLL), mixed cell type. Although the possibility of Richter’s transformation could not be ruled out, clinical, laboratory, and radiologic findings did not support this diagnosis (data not shown).
Patients with aCLL may experience more aggressive disease and shortened survival. Also, as was seen in this case, aCLL has been associated with poor prognostic indicators such as unmutated IgVH, CD38+, ZAP70+, and trisomy 12. Digital microscopy is a rapid and inexpensive screening tool that improves the ability to identify aCLL patients. An experienced morphologist can quickly compare/contrast and classify variant lymphocytes as they are presented on a wide-screen monitor. The images are archived for a second review if needed and comparison with previous or subsequent results.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal