In this issue of Blood, Kim et al and Gardenghi et al present companion reports exploring the physiology of the anemia of critical illness following intraperitoneal injection of heat-killed Brucella abortus bacteria into mice.1,2
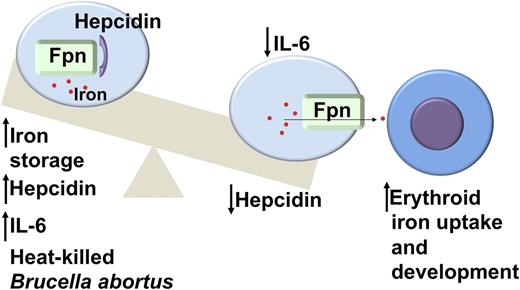
A model of the pathophysiology of the anemia of inflammation based on the findings in Kim et al and Gardenghi et al.1,2 Injection of heat-killed B abortus stimulates an inflammatory response including increased production of hepcidin and IL-6. Hepcidin binds to the iron exporter ferroportin resulting in internalization of the protein, increased macrophage iron storage, and subsequent hypoferremia. Recovery from the inflammatory response lowers hepcidin and IL-6 levels leading to increased release of iron from the macrophages to the developing erythrocytes and relief of the block in erythroid development. Fpn, ferroportin.
A model of the pathophysiology of the anemia of inflammation based on the findings in Kim et al and Gardenghi et al.1,2 Injection of heat-killed B abortus stimulates an inflammatory response including increased production of hepcidin and IL-6. Hepcidin binds to the iron exporter ferroportin resulting in internalization of the protein, increased macrophage iron storage, and subsequent hypoferremia. Recovery from the inflammatory response lowers hepcidin and IL-6 levels leading to increased release of iron from the macrophages to the developing erythrocytes and relief of the block in erythroid development. Fpn, ferroportin.
Anemia is a common phenomenon in the critically ill that is often attributed to frequent phlebotomy and bleeding; however, several studies have demonstrated that even previously healthy patients rapidly develop many of the features of the anemia of chronic disease when hospitalized in the intensive care unit. These findings include low serum iron levels, low ratios of serum iron to total iron-binding capacity, increased serum ferritin levels, inappropriately low levels of erythropoietin, and elevated measures of inflammatory markers, such as C-reactive protein.3 As demonstrated in the CRIT study, Anemia and Blood Transfusion in the Critically Ill, an observational cohort analysis of 4892 patients in intensive care units across the United States,4 mean hemoglobin levels decreased over 30 days despite the administration of blood transfusions. Furthermore, a nadir hemoglobin <9 g/dL was an independent predictor of increased mortality and length of stay. For these reasons, it is important to understand the effects of acute, severe inflammation on iron homeostasis and erythropoiesis.
Our understanding of anemia of inflammation has been revolutionized by the discovery of the peptide hormone, hepcidin. Hepcidin (also known as HAMP or HAMP1 in mice) functions primarily to modulate iron uptake from enterocytes to the bloodstream and the release of iron from macrophages to developing erythrocytes. The physiological stimuli of iron overload or inflammation each induce hepcidin’s transcription.5 Previous studies indicate that inflammation stimulates production of interleukin-6 (IL-6),6 which increases hepcidin transcription by activating the signal transducer and activator of transcription (Stat) signaling pathway.7 Recent efforts are evaluating the role of antibodies against IL-6 or hepcidin to treat the anemia of inflammation.8,9 Conversely, molecules that increase hepcidin expression via Stat activation are being developed as treatments for iron overload syndromes.10
Previous mouse models utilizing infectious or noninfectious triggers of inflammation have produced only mild and variable anemia.11 What is particularly appealing about the killed B abortus model of anemia of inflammation is that the hemoglobin level in the treated mice consistently decreased by 50% 14 days after a single intraperitoneal injection. Furthermore, erythropoiesis gradually recovered following the injection, just as human patients may recover from the insult of a critical illness, such as sepsis. The ease and consistency of the killed B abortus model facilitated an in-depth evaluation of the hematologic effects of inflammation over time and in multiple mouse strains. Both studies found evidence of several features of the anemia of critical illness including an increase in hepcidin expression and serum iron levels 6 hours following the inflammatory injection. Both studies implicated hepcidin as the mediator of the hypoferremia and anemia, as injection of the killed B abortus bacteria in Hepcidin-knockout mice produced a blunted effect. Gardenghi et al further evaluated the effects in IL-6–knockout mice and found that IL-6 deficiency protected against hypoferremia and anemia. Erythropoietic differences were observed between the hepcidin-knockout and IL-6–knockout mice: hepcidin-deficient animals exhibited increased splenic erythropoiesis immediately following the insult, while IL-6–knockout mice exhibited faster recovery of bone marrow erythropoiesis. One of the interesting findings of both studies, which is not completely understood, is that the erythrocytes exhibited shorter lifespans following injection of killed B abortus. Kim et al observed schistocytes in the peripheral blood of the injected animals and microthrombi in the liver and kidney, consistent with microangiopathic hemolytic anemia, while flow cytometry analysis by Gardenghi et al supports a role for hemophagocytosis. Either of these phenomena could occur in patients with severe inflammation and contribute to the anemia of critical illness.
The implication of these studies is that pharmacologic agents that decrease hepcidin expression may prevent the anemia of inflammation; however, it is not known whether this would improve morbidity or mortality in human patients. Arguing for a protective effect of the anemia of inflammation, hepcidin-knockout mice exhibited significantly impaired survival compared with wild-type controls following injection of killed B abortus.1 Nonetheless, these studies improve our understanding of the pathophysiology of anemia in patients with severe inflammation or critical illness and may form the basis for further studies to develop new agents to treat this at-risk population.
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal