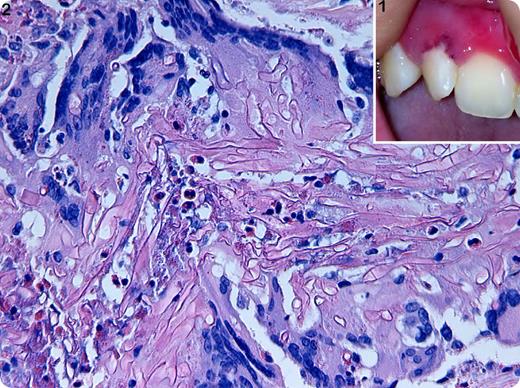
An 18-y-old woman diagnosed of lymphoblastic T-cell lymphoma underwent a second allogenic stem cell transplantation (CD3/CD19 depleted Haploidentical) for relapsing lymphoma. She achieved a third complete remission. Five months later she was admitted for a neutropenic fever. A urinary infection was diagnosed and resolved with broad-spectrum antibiotic. Bone marrow aspiration showed isolated myeloid aplasia. After 4 wk of persistent neutropenia (<100 neutrophils/µL), the fever reappeared. A small ulcerative lesion was observed in the upper maxillary zone (Panel 1). A paranasal sinuses and facial computer tomography was performed. It showed normal features. Zygomicetes spp was isolated in an exudate culture in the lesion itself. A diagnosis of mucormycosis was assumed. The patient underwent a partial maxillectomy and a double antifungal treatment together with posaconazol and liposomal amphotericin. The final histopathological diagnosis was proven by a surgical specimen. Histological findings showed large amounts of necrotic tissue and fungal aseptate and branched Periodic acid-Schiff–positive hyphae, compatible with the diagnosis of invasive mucormycosis (Panel 2).
Successful management of this potentially lethal infection requires early recognition of disease, especially in immunocompromised patients. Highly aggressive surgical approaches and selective medical treatment are paramount to avoid high morbidity and mortality related to this disease.
An 18-y-old woman diagnosed of lymphoblastic T-cell lymphoma underwent a second allogenic stem cell transplantation (CD3/CD19 depleted Haploidentical) for relapsing lymphoma. She achieved a third complete remission. Five months later she was admitted for a neutropenic fever. A urinary infection was diagnosed and resolved with broad-spectrum antibiotic. Bone marrow aspiration showed isolated myeloid aplasia. After 4 wk of persistent neutropenia (<100 neutrophils/µL), the fever reappeared. A small ulcerative lesion was observed in the upper maxillary zone (Panel 1). A paranasal sinuses and facial computer tomography was performed. It showed normal features. Zygomicetes spp was isolated in an exudate culture in the lesion itself. A diagnosis of mucormycosis was assumed. The patient underwent a partial maxillectomy and a double antifungal treatment together with posaconazol and liposomal amphotericin. The final histopathological diagnosis was proven by a surgical specimen. Histological findings showed large amounts of necrotic tissue and fungal aseptate and branched Periodic acid-Schiff–positive hyphae, compatible with the diagnosis of invasive mucormycosis (Panel 2).
Successful management of this potentially lethal infection requires early recognition of disease, especially in immunocompromised patients. Highly aggressive surgical approaches and selective medical treatment are paramount to avoid high morbidity and mortality related to this disease.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal