Key Points
Several common and rare VWF missense variants contribute to phenotypic differences in VWF and FVIII among African Americans.
Next-generation sequencing technology and improved genotype imputation can contribute to molecular genetics of VWD-related phenotypes.
Abstract
Several rare European von Willebrand disease missense variants of VWF (including p.Arg2185Gln and p.His817Gln) were recently reported to be common in apparently healthy African Americans (AAs). Using data from the NHLBI Exome Sequencing Project, we assessed the association of these and other VWF coding variants with von Willebrand factor (VWF) and factor VIII (FVIII) levels in 4468 AAs. Of 30 nonsynonymous VWF variants, 6 were significantly and independently associated (P < .001) with levels of VWF and/or FVIII. Each additional copy of the common VWF variants encoding p.Thr789Ala or p.Asp1472His was associated with 6 to 8 IU/dL higher VWF levels. The VWF variant encoding p.Arg2185Gln was associated with 7 to 13 IU/dL lower VWF and FVIII levels. The type 2N-related VWF variant encoding p.His817Gln was associated with 17 IU/dL lower FVIII level but normal VWF level. A novel, rare missense VWF variant that predicts disruption of an O-glycosylation site (p.Ser1486Leu) and a rare variant encoding p.Arg2287Trp were each associated with 30 to 40 IU/dL lower VWF level (P < .001). In summary, several common and rare VWF missense variants contribute to phenotypic differences in VWF and FVIII among AAs.
Introduction
Von Willebrand factor (VWF) is a multimeric plasma glycoprotein that plays an important role in hemostasis and thrombosis.1 VWF adheres to sites of vascular injury, binds platelets, and stabilizes factor VIII (FVIII) in the circulation. High VWF levels are associated with increased risk of venous thrombosis, myocardial infarction, and ischemic stroke.2,3 Conversely, deficiency of VWF is associated with bleeding and a diagnosis of von Willebrand disease (VWD), the most common inherited bleeding disorder in humans.4
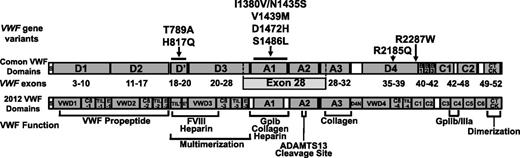
The human VWF gene is located on chromosome 12p13.3, spans 178 kb, and is composed of 52 exons ranging in size from 40 bases to 1.4 kb (exon 28).5 The translated pre–pro-VWF molecule contains 2813 amino acids, comprising a 22-residue signal peptide, a 741–amino acid propeptide, and a highly glycosylated 2050–amino acid mature VWF subunit, also known as VWF antigen, composed of repeated VWF domains commonly annotated A to D arranged in the order D1-D2-D′-D3-A1-A2-A3-D4-B1-B2-B3-C1-C2-CK (Figure 1 top). The architecture of these VWF domains is the result of complex duplications, and a recent revised VWF domain annotation based upon sequence homology and structure studies has been published6 (Figure 1 bottom). VWF mutations can be detected in many type 1 VWD cases and in nearly all type 2 and 3 patients.5,7 Type 2 VWD variants, characterized by defects in multimerization, proteolysis, or interaction with VWF ligands (platelets, collagen, or FVIII), tend to be localized to particular functional domains encoded by VWF exons 18 to 25 (D′-D3 domains, type 2N) exon 28 (A1-A2 domains, types 2A, 2B, and 2M), and exons 11 to 16, 24 to 26, and 51 to 52 (type 2A). On the other hand, type 1 and type 3 VWD mutations occur throughout the VWF gene.
Scale schematic of VWF missense variants associated with levels of VWF or FVIII levels in African Americans (AAs). The location of each of VWF variants with significant univariate associations with VWF and/or FVIII levels in AAs are indicated by arrows to the corresponding commonly annotated VWF domain (top). An alignment with the recently revised VWF domain annotation6 is also shown (bottom). Two variants, I1380V and N1435S, are in strong LD (r2 = 0.89) and are therefore represented together.
Scale schematic of VWF missense variants associated with levels of VWF or FVIII levels in African Americans (AAs). The location of each of VWF variants with significant univariate associations with VWF and/or FVIII levels in AAs are indicated by arrows to the corresponding commonly annotated VWF domain (top). An alignment with the recently revised VWF domain annotation6 is also shown (bottom). Two variants, I1380V and N1435S, are in strong LD (r2 = 0.89) and are therefore represented together.
Two-thirds of phenotypic variation in VWF level is attributable to heritable factors, with one-third of the heritable variance due to the influence of ABO blood group.8,9 Common VWF polymorphisms, such as the missense variant rs1063857 (encoding p.Thr789Ala), also influence VWF levels.10,11 VWF antigen (VWF:Ag) and FVIII coagulation activity levels (FVIII:C) are higher in AAs than in European Americans (EAs), and this difference is not explained by known differences in ABO allele frequencies.12-15 The ratio of VWF activity (ristocetin cofactor activity) to VWF:Ag is lower among AAs than EAs.15,16 Consequently, AAs are diagnosed more frequently with the qualitative type 2M variant of VWD.16
Until recently, molecular genetic analyses of VWD and population genomic studies of VWF were largely confined to populations of European descent. Two recent analyses of population-based sequencing data demonstrated considerable ethnic diversity in coding sequence variation at the VWF locus.17,18 Several VWF missense variants, previously reported in EAs as rare VWD-causing mutations (including p.Met740Ile, p.His817Gln, and p.Arg2185Gln), were considerably more common (minor allele frequencies [MAF] = 10%-15%) in AA.17,18 This observation, together with the lack of association between these variants and VWF-related phenotypes in 66 AAs,17 called into question whether these VWF missense variants are indeed functional or pathogenic. To further address this question, we used VWF exonic sequence data from the NHLBI Exome Sequencing Project to assess the association of coding variants with VWF:Ag and FVIII:C levels in a large population-based sample of AAs.
Methods
Subjects
Participants included 4468 self-identified AAs with VWF and/or FVIII measurements from 4 population-based cohorts: the Atherosclerosis Risk in Communities (ARIC), Coronary Artery Risk Development in Young Adults (CARDIA), Multi-Ethnic Study of Atherosclerosis (MESA), and Women’s Health Initiative (WHI). Clinical information was collected by self-report and in-person examination. Detailed descriptions and VWF and FVIII laboratory methods for each cohort are provided in supplemental Methods. The 4468 AAs included 595 participants with exome sequence data and 3873 with imputed genotypes using preexisting GWAS data, as described below. In accordance with the Declaration of Helsinki, all participants provided written informed consent as approved by local institutional review boards.
Exome sequencing and VWF coding variant identification
We used VWF coding sequence data derived from the NHLBI Exome Sequencing Project (ESP).19 Through ESP, 15 336 genes were sequenced at high coverage (median depth >100×) in a total of 6515 unrelated individuals (4298 EAs and 2217 AAs) from 19 different studies. Library construction, exome capture, sequencing, mapping, calling, and filtering were carried out as described previously.20,21 Exome sequence data were aligned to NCBI human reference GRCh37. The 6515 ESP participants were selected based on a variety of cardiovascular and pulmonary phenotypes (coronary heart disease, stroke, diabetes, asthma, COPD, acute lung injury, pulmonary artery hypertension, cystic fibrosis, and extremes of blood pressure, body mass, or low-density lipoprotein cholesterol). The sample for exome sequencing included a total of 1455 AAs from the ARIC, CARDIA, MESA, and WHI cohorts. Of the 1455 AA ESP participants with exome sequence data, 595 with VWF:Ag and FVIII:C phenotype measurements are included in the current analysis.
For the region on chromosome 12p13.31 containing VWF (nucleotides 6 058 040-6 233 836), the average sample read depth was 77× (range 1×-374×) in AAs. Coverage included the entire coding sequence and exon-intron boundaries. Sequence data were aligned with VWF reference sequence NM_000552.3. The VWF pseudogene sequence on chromosome 22 (position 17 161,397-17 185,967 using Build 37) shares 97% sequence homology with exons 23 to 34 of the VWF structural gene. We computed the genome mappability score profile (a weighted probability that any read could be unambiguously mapped to a given position)22 under a variety of read-length models and demonstrated that the entire VWF structural gene exonic sequence could be reliably mapped (data not shown).
There were 409 VWF variant sites in AAs. Most of these sites were singletons (170, or 42%) and doubletons (42, or 10%). Of the 409 AA variant sites, 147 were infrequent or common (MAF > 0.1%). Additional details can be found at http://evs.gs.washington.edu/EVS/. The VWF coding variants identified through ESP are also summarized in supplemental Table 1.
Imputation of VWF coding variant genotypes into a larger AA sample
Using an imputation procedure, we probabilistically determined the genotypes for the 147 VWF missense variants with MAF > 0.1% that were identified through exome sequencing in a larger sample of 3873 AAs with VWF:Ag and/or FVIII:C levels and Affymetrix 6.0 genome-wide genotyping data from the parent ARIC, CARDIA, MESA, and WHI cohorts. We used as our imputation reference panel a subset of 2163 ESP participants (1692 AAs, 471 EAs) with exome sequence data who had been genotyped on Affymetrix 6.0 GWAS platform. Variant- and sample-level processing, quality control, and filtering of the Affymetrix 6.0 genotype data were performed as described previously.23,24 The target and reference panels were prephased using BEAGLE.25 We then used minimac26 to probabilistically impute genotypes, as described previously.24
Sequence variants were excluded at the calling stage for a read depth <10×. Prior to data analysis, single-nucleotide variants (SNVs) were additionally excluded on the basis of imputation quality. We used the imputation quality metric Rsq, which ranges from a value of 1 (no genotype uncertainty) to 0 (complete uncertainty). Using previously defined MAF-based thresholds, SNVs passing the quality-control threshold had an average Rsq of ≥0.8.24 Of the total of 147 SNV from the VWF gene with MAF > 0.1% identified by exome sequencing in AA, 114 SNV (30 missense, 28 synonymous, and 56 intronic) were successfully imputed.
Statistical analysis
Association analyses of 30 VWF missense variants with VWF and FVIII levels were performed assuming an additive genetic model. We used linear regression, with natural-log–transformed VWF:Ag and FVIII:C level as the dependent variable, with adjustment for age, sex, and the top 2 principal components derived from analysis of the GWAS data.27 These principal components represent summary measures of genetic ancestry and thereby correct for any cryptic relatedness or population stratification. For the analyses using sequence data, we additionally controlled for sequence capture target and primary ESP phenotype in order to correct for any bias due to heterogeneity in sequencing technology or sampling strategy, respectively. Allelic dosage at each variant (a value between 0.0 and 2.0 calculated based on the probability of each of the 3 possible imputed genotypes) was the independent variable in each linear regression model. This analytic approach provides an efficient, powerful, and robust alternative to methods that fully account for imputed genotype uncertainty.28 In these analyses, the β coefficient derived from each linear regression model approximates the change in natural-log–transformed VWF:Ag and FVIII:C per each additional copy of the variant allele (also referred to as the “effect allele”). To provide more clinically relevant mean VWF or FVIII effect sizes, β coefficients and standard errors per each additional copy of the minor allele were also reported for corresponding regression models using untransformed VWF:Ag or FVIII:C. To allow comparison of consistency of results between cohorts, we analyzed each study separately and combined the results using meta-analysis, as described in supplemental Methods. Since 30 nonsynonymous coding SNVs were tested, we used a conservative Bonferroni-adjusted threshold of P < .05/30 (.0017) to declare statistical significance.
Allelic correlation as a measure of linkage disequilibrium (LD) between pairs of polymorphic sites was calculated as r2. Haplotypes were inferred from ESP AA sequence data using the haplotype reconstruction algorithm and haplotype association analyses were performed using HAPLO.STAT implemented in the R statistical computing language.29 We assessed the potential functional impact of each VWF missense variant on VWF structure/function using in silico prediction methods described in detail in supplemental Methods.
Results
The characteristics of the AA participants by cohort are summarized in Table 1. The overall correlation between VWF and FVIII levels was 0.70. Significant differences between cohorts were observed for age, sex, body mass index, and smoking status. Differences in mean VWF:Ag and FVIII:C levels between cohorts most likely reflect differences in demographic characteristics as well as interassay variability between laboratories (see supplemental Methods).
Characteristics of 4468 AA participants by cohort
| Study . | ARIC . | CARDIA . | MESA . | WHI . | Total* . | P value for differences between cohorts . |
|---|---|---|---|---|---|---|
| Sample size | 2354 | 353 | 1607 | 154 | 4468 | — |
| Age, y (SD) | 53.3 (5.8) | 24.9 (4.4) | 62.2 (10.1) | 65.2 (6.5) | 54.8 (12.4) | <.0001 |
| Female (%) | 63 | 61 | 54 | 100 | 61 | <.0001 |
| BMI (SD) | 29.7 (6.1) | 25.4 (5.7) | 29.9 (5.5) | 31.3 (5.1) | 29.3 (6.2) | <.0001 |
| Current smoker | 28.9% | 33.9% | 24.7% | 29.4% | 27.8% | <.0001 |
| VWF antigen, IU/dL (SD) | 135 (58) | 102 (42) | 154 (62) | 123 (66) | 132 (58) | <.0001 |
| FVIII activity, IU/dL (SD) | 148 (48) | 102 (38) | 115 (47) | 123 (63) | 128 (15) | <.0001 |
| FVIII/VWF ratio | 1.18 (0.33) | 1.12 (0.53) | 1.20 (0.40) | 1.15 (0.62) | 1.18 (0.37) | .02 |
| Ristocetin cofactor activity | NA | 92 (40) | NA | NA | 92 (40) | — |
| Study . | ARIC . | CARDIA . | MESA . | WHI . | Total* . | P value for differences between cohorts . |
|---|---|---|---|---|---|---|
| Sample size | 2354 | 353 | 1607 | 154 | 4468 | — |
| Age, y (SD) | 53.3 (5.8) | 24.9 (4.4) | 62.2 (10.1) | 65.2 (6.5) | 54.8 (12.4) | <.0001 |
| Female (%) | 63 | 61 | 54 | 100 | 61 | <.0001 |
| BMI (SD) | 29.7 (6.1) | 25.4 (5.7) | 29.9 (5.5) | 31.3 (5.1) | 29.3 (6.2) | <.0001 |
| Current smoker | 28.9% | 33.9% | 24.7% | 29.4% | 27.8% | <.0001 |
| VWF antigen, IU/dL (SD) | 135 (58) | 102 (42) | 154 (62) | 123 (66) | 132 (58) | <.0001 |
| FVIII activity, IU/dL (SD) | 148 (48) | 102 (38) | 115 (47) | 123 (63) | 128 (15) | <.0001 |
| FVIII/VWF ratio | 1.18 (0.33) | 1.12 (0.53) | 1.20 (0.40) | 1.15 (0.62) | 1.18 (0.37) | .02 |
| Ristocetin cofactor activity | NA | 92 (40) | NA | NA | 92 (40) | — |
Mean (SD) values are shown for age, body mass index, VWF antigen, FVIII activity, FVIII/VWF ratio, and ristocetin cofactor activity.
BMI, body mass index; NA, not available; SD, standard deviation.
Of the total of 4468 AA participants, VWF levels were measured in 2989 and FVIII levels were measured in 4430. Both measurements were available in 2951 participants. Ristocetin cofactor activity was measured in 165 CARDIA participants.
Of the 30 VWF missense variants, the consensus prediction for 7 were predicted to be deleterious and 23 were predicted to be neutral, though there was considerable heterogeneity between each of the individual prediction methods (supplemental Table 2). We determined pairwise LD using the full set of Exome Sequencing Project AA (supplemental Figure 1). Only 2 pairs of variants showed moderate allelic correlation or LD (defined as r2 > 0.5): rs11063987 (p.Ser1435Asn) with rs11063988 (p.Ile1380Val) (r2 = 0.89) and rs75645183 (p.Asp837Ala) with rs78302129 (p.Ser1725Pro) (r2 = 0.73). p.Arg2185Gln, p.Asp1472His, and p.Ser1435Asn/Ile1380Val were in weak LD with one another (pairwise r2 in the range of 0.1-0.2).
Association results for VWF missense variants
A total of 9 of the 30 VWF missense variants tested (30%) were significantly (P < .0017) associated with VWF:Ag and/or FVIII:C (Table 2). A complete list of association results for all 30 missense variants is provided in supplemental Table 3. There was little evidence of heterogeneity of results (supplemental Table 3), and effect sizes were relatively consistent across cohorts (supplemental Figure 2). A total of 6 of the 9 variants were common (MAF > 5%) and 3 were infrequent or rare (MAF < 1%) in AA. The rare variant encoding p.Ser1486Leu disrupts a predicted O-linked glycosylation site adjacent to the A1 domain but has not been reported previously.
VWF missense variants associated with VWF antigen and/or FVIII coagulant activity in AAs
| Variant (chromosome/BP) . | Rs number . | Annotation . | EAF AA . | EAF EA* . | Imputation quality (Rsq)† . | Functional prediction‡ . | N . | VWF β (SE) . | Ln(VWF) β (SE) . | Ln(VWF) P value . | N . | FVIII β (SE) . | Ln(FVIII) β (SE) . | Ln(FVIII) P value . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| chr12:6153534 | 1063856 | Thr789Ala | 0.58 | 0.3600 | 1.00 | Benign | 2976 | 8.62 (1.56) | 0.0664 (0.0109) | 1.05E-09 | 4432 | 7.22 (1.36) | 0.0377 (0.0078) | 1.24E-06 |
| chr12:6145649 | 57950734 | His817Gln | 0.11 | 0.0003 | 0.97 | Deleterious | 2976 | −4.74 (2.57) | −0.0317 (0.018) | .078 | 4432 | −17.8 (2.23) | 0.1205 (0.0127) | 1.77E-21 |
| chr12:6128446 | 11063988 | Ile1380Val | 0.11 | 0.00035 | 0.82 | Benign | 2934 | 6.33 (2.71) | 0.059 (0.0188) | .0017 | 4360 | 9.39 (2.42) | −0.0641 (0.0137) | 2.74E-06 |
| chr12:6128280 | 11063987 | Asn1435Ser | 0.11 | 0.00023 | 0.85 | Benign | 2976 | 6.05 (2.50) | 0.0555 (0.0186) | .0028 | 4432 | 9.72 (2.41) | 0.0647 (0.0135) | 1.71E-06 |
| chr12:6128269 | 150077670 | Met1439Val | 0.0044 | <1/12000 | 0.90 | Benign | 2543 | −34.5 (12.7) | −0.3279 (0.0958) | .00062 | 3838 | −15.6 (11.0) | −0.1186 (0.0665) | .074 |
| chr12:6128170 | 1800383 | Asp1472His | 0.393 | 0.066 | 0.85 | Benign | 2976 | 5.48 (1.66) | 0.038 (0.0125) | .0010 | 4432 | 2.52 (1.50) | 0.0183 (0.0095) | .055 |
| chr12:6128127 | 149424724 | Ser1486Leu | 0.008 | 0.0001 | 0.75 | Benign | 2967 | −40.3 (10.0) | −0.3585 (0.0677) | 1.18E-07 | 4420 | −9.68 (8.84) | −0.1200 (0.0494) | .015 |
| chr12:6103072 | 76342212 | Arg2185Gln | 0.19 | 0.0015 | 0.97 | Benign | 2973 | −13.1 (2.03) | −0.1013 (0.0141) | 6.24E-13 | 4428 | −13.1 (1.78) | −0.0856 (0.0101) | 1.86E-17 |
| chr12:6094771 | 61750625 | Arg2287Trp | 0.00763 | 0 | 0.70 | Deleterious | 2976 | −39.6 (9.71) | −0.3064 (0.0634) | 1.33E-06 | 4432 | −15.2 (8.78) | −0.1108 (0.0481) | .021 |
| Variant (chromosome/BP) . | Rs number . | Annotation . | EAF AA . | EAF EA* . | Imputation quality (Rsq)† . | Functional prediction‡ . | N . | VWF β (SE) . | Ln(VWF) β (SE) . | Ln(VWF) P value . | N . | FVIII β (SE) . | Ln(FVIII) β (SE) . | Ln(FVIII) P value . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| chr12:6153534 | 1063856 | Thr789Ala | 0.58 | 0.3600 | 1.00 | Benign | 2976 | 8.62 (1.56) | 0.0664 (0.0109) | 1.05E-09 | 4432 | 7.22 (1.36) | 0.0377 (0.0078) | 1.24E-06 |
| chr12:6145649 | 57950734 | His817Gln | 0.11 | 0.0003 | 0.97 | Deleterious | 2976 | −4.74 (2.57) | −0.0317 (0.018) | .078 | 4432 | −17.8 (2.23) | 0.1205 (0.0127) | 1.77E-21 |
| chr12:6128446 | 11063988 | Ile1380Val | 0.11 | 0.00035 | 0.82 | Benign | 2934 | 6.33 (2.71) | 0.059 (0.0188) | .0017 | 4360 | 9.39 (2.42) | −0.0641 (0.0137) | 2.74E-06 |
| chr12:6128280 | 11063987 | Asn1435Ser | 0.11 | 0.00023 | 0.85 | Benign | 2976 | 6.05 (2.50) | 0.0555 (0.0186) | .0028 | 4432 | 9.72 (2.41) | 0.0647 (0.0135) | 1.71E-06 |
| chr12:6128269 | 150077670 | Met1439Val | 0.0044 | <1/12000 | 0.90 | Benign | 2543 | −34.5 (12.7) | −0.3279 (0.0958) | .00062 | 3838 | −15.6 (11.0) | −0.1186 (0.0665) | .074 |
| chr12:6128170 | 1800383 | Asp1472His | 0.393 | 0.066 | 0.85 | Benign | 2976 | 5.48 (1.66) | 0.038 (0.0125) | .0010 | 4432 | 2.52 (1.50) | 0.0183 (0.0095) | .055 |
| chr12:6128127 | 149424724 | Ser1486Leu | 0.008 | 0.0001 | 0.75 | Benign | 2967 | −40.3 (10.0) | −0.3585 (0.0677) | 1.18E-07 | 4420 | −9.68 (8.84) | −0.1200 (0.0494) | .015 |
| chr12:6103072 | 76342212 | Arg2185Gln | 0.19 | 0.0015 | 0.97 | Benign | 2973 | −13.1 (2.03) | −0.1013 (0.0141) | 6.24E-13 | 4428 | −13.1 (1.78) | −0.0856 (0.0101) | 1.86E-17 |
| chr12:6094771 | 61750625 | Arg2287Trp | 0.00763 | 0 | 0.70 | Deleterious | 2976 | −39.6 (9.71) | −0.3064 (0.0634) | 1.33E-06 | 4432 | −15.2 (8.78) | −0.1108 (0.0481) | .021 |
Linear regression models were initially run with natural-log–transformed VWF and FVIII level as the dependent variable, with adjustment for age, sex, and genetic ancestry (as inferred from principal component analysis), as described under “Methods.” The β coefficient corresponds to the mean difference in natural-log–transformed VWF or FVIII between an individual carrying 1 copy of the “effect allele” compared with individuals carrying 0 copies of the effect allele. The effect allele refers to the second amino acid under “Annotation.” Effect allele frequency indicates the frequency of the effect allele in AAs and EAs. To provide more clinically relevant mean VWF or FVIII effect sizes, β coefficients and standard errors per each additional copy of the minor allele were also reported for corresponding regression models using untransformed VWF or FVIII.
BP, base pair; EAF, effect allele frequency; SE, standard error.
Allele frequency data in EAs from NHLBI Exome Sequencing Project (ESP) Exome Variant Server (evs.gs.washington.edu/EVS/).
Imputation quality Rsq is an estimate of the correlation between the imputed genotype and the actual genotype and serves as a measure of imputation accuracy.
Functional prediction of the potential impact of the VWF missense variant was determined using the algorithm Condel (CONsensus DELeteriousness score of nonsynonymous single nucleotide variants), as described in supplemental Methods and in supplemental Table 2.
Each additional copy of the rs1063856 (p.Thr789Ala) G allele (Ala789) was associated with 9 IU/dL higher VWF:Ag and 7 IU/dL higher FVIII:C levels. Each additional copy of the rs2229446 (p.Arg2185Gln) minor allele was associated with 13 IU/dL lower VWF:Ag and FVIII:C levels. rs57950734 (p.His817Gln) minor allele was associated with a significant 18 IU/dL per allele decrease in FVIII:C level but had no significant association with VWF:Ag level. Three common exon 28 coding variants (p.Ile1380Val, p.Asn1435Ser, and p.Asp1472His) were associated with 5 to 6 IU/dL higher VWF:Ag levels; p.Ile1380Val and p.Asn1435Ser were additionally associated with 9 and 10 IU/dL higher FVIII:C levels, respectively. Three rare missense variants—rs150077870 (p.Met1439Val; MAF = 0.4%), rs149424724 (p.Ser1486Leu; MAF = 0.8%), and rs61750625 (p.Arg2287Trp; MAF = 0.7%)—were each associated with lower VWF:Ag level but had no significant association with FVIII:C level. The presence of a single copy of the p.Met1439Val, p.Ser1486Leu, or p.Arg2287Trp variants was associated with an average per allele difference in VWF:Ag level in the range of 35 to 40 IU/dL.
Since AAs have a lower VWF ristocetin cofactor activity to VWF antigen ratio compared with EAs,13,14 we further evaluated 5 exon 28 A1 domain variants in the subset of 165 CARDIA AA participants who had VWF antigen and ristocetin cofactor activity measured. There was no evidence of association between any of these variants of the ratio of VWF activity to VWF antigen (supplemental Table 4), although power to detect an association was limited by the small sample size.
Assessment of independent effect of each missense variant on VWF and FVIII levels
Due to the strong LD between p.Ile1380Val and p.Asn1435Ser, the effects of these 2 SNV on VWF:Ag and FVIII:C levels are collinear and therefore indistinguishable. We assessed the independent effects of each of the remaining 8 missense variants on VWF or FVIII phenotype by performing a multivariable regression model with simultaneous adjustment for the remaining 7 variants (Table 3). In this multivariable model, the 8 SNVs in aggregate explained 3.3% of the overall VWF:Ag phenotypic variance and 2.7% of the overall FVIII:C phenotypic variance. When accounting for the joint effects of the remaining missense variants, (1) the common p.Thr789Ala variant remained independently associated with higher VWF:Ag and FVIII:C; (2) p.Arg2185Gln remained independently associated with lower VWF:Ag and FVIII:C levels; (3) p.His817Gln remained independently associated with lower FVIII:C level; (4) the rare p.Arg2287Trp variant remained independently associated with lower VWF:Ag and FVIII:C levels; and (5) p.Ser1486Asn remained independently associated with VWF:Ag level (all P < .0017). Accounting for the effects of the remaining variants altered the magnitude and phenotypic patterns of association for variants located within exon 28. Specifically, p.Asp1472His became more strongly associated with higher VWF:Ag level, while the associations of p.Asn1435Ser or p.Ile1380Val and p.Met1439Val with VWF:Ag and FVIII:C levels weakened and were no longer statistically significant at P < .0017.
Multivariate regression model of VWF missense variants and VWF antigen and FVIII coagulation activity
| Variant . | Rs number . | Annotation . | VWF β (SE) . | VWF P value . | FVIII β (SE) . | FVIII P value . |
|---|---|---|---|---|---|---|
| chr12:6153534 | 1063856 | Thr789Ala | 5.92 (1.48) | 6.4E-05 | 7.68 (1.30) | 4.4E-09 |
| chr12:6145649 | 57950734 | His817Gln | −1.48 (2.63) | .57 | −16.72 (2.36) | 1.6E-12 |
| chr12:6128280 | 11063987 | Asn1435Ser | .087 (2.70) | .97 | 6.60 (2.45) | .007 |
| chr12:6128269 | 150077670 | Met1439Val | −20.75 (13.09) | .11 | −3.06 (11.09) | .78 |
| chr12:6128446 | 11063988 | Asp1472His | 7.63 (1.87) | 4.8E-05 | 4.55 (1.70) | .007 |
| chr12:6128127 | 149424724 | Ser1486Leu | −32.1 (9.07) | 4.1E-04 | −1.92 (8.17) | .81 |
| chr12:6103072 | 76342212 | Arg2185Gln | −12.7 (2.16) | 4.54E-09 | −7.02 (1.94) | 3.1E-04 |
| chr12:6094771 | 61750625 | Arg2287Trp | −41.5 (8.57) | 1.3E-06 | −21.2 (7.91) | .007 |
| Variant . | Rs number . | Annotation . | VWF β (SE) . | VWF P value . | FVIII β (SE) . | FVIII P value . |
|---|---|---|---|---|---|---|
| chr12:6153534 | 1063856 | Thr789Ala | 5.92 (1.48) | 6.4E-05 | 7.68 (1.30) | 4.4E-09 |
| chr12:6145649 | 57950734 | His817Gln | −1.48 (2.63) | .57 | −16.72 (2.36) | 1.6E-12 |
| chr12:6128280 | 11063987 | Asn1435Ser | .087 (2.70) | .97 | 6.60 (2.45) | .007 |
| chr12:6128269 | 150077670 | Met1439Val | −20.75 (13.09) | .11 | −3.06 (11.09) | .78 |
| chr12:6128446 | 11063988 | Asp1472His | 7.63 (1.87) | 4.8E-05 | 4.55 (1.70) | .007 |
| chr12:6128127 | 149424724 | Ser1486Leu | −32.1 (9.07) | 4.1E-04 | −1.92 (8.17) | .81 |
| chr12:6103072 | 76342212 | Arg2185Gln | −12.7 (2.16) | 4.54E-09 | −7.02 (1.94) | 3.1E-04 |
| chr12:6094771 | 61750625 | Arg2287Trp | −41.5 (8.57) | 1.3E-06 | −21.2 (7.91) | .007 |
Independent effects of each of the 8 missense variants on VWF or FVIII phenotype were evaluated by performing a multivariable regression model adjusted for age, sex, genetic ancestry (as inferred from principal component analysis) and the 7 remaining missense variants. The β coefficient corresponds to the mean difference in natural-log–transformed VWF or FVIII between an individual carrying 1 copy of the “effect allele” compared with individuals carrying 0 copies of the effect allele.
SE, standard error.
We further assessed the exon 28 region by performing haplotype analysis of p.Ile1380Val, p.Asn1435Ser, p.His1472Asp, and p.Arg2185Gln in the subset of AAs with exome sequence and phenotypic data (Table 4). Compared with the most common (reference) haplotype (frequency = 0.50), the haplotype containing the His1472 variant alone (frequency = 0.21) was associated with higher VWF:Ag (P = .017) and FVIII:C levels (P = .010). In contrast, the haplotype containing Val1380/Ser1435/His1472 (frequency = 0.10) showed no evidence of phenotypic association with either VWF:Ag or FVIII:C level.
Association of VWF exon 28 haplotypes with VWF antigen and FVIII levels in AAs (N = 612)
| Haplotype . | VWF SNP . | . | VWF level . | FVIII level . | |||||
|---|---|---|---|---|---|---|---|---|---|
| Ile1380Val . | Asn1435Ser . | Asp1472His . | Arg2185Gln . | Freq . | β (SE) . | P value . | β (SE) . | P value . | |
| H1 | 0 | 0 | 0 | 0 | 0.500 | Referent | — | Referent | — |
| H2 | 0 | 0 | 1 | 0 | 0.210 | 13.7 (5.7) | .017 | 11.3 (4.4) | .010 |
| H3 | 0 | 0 | 1 | 1 | 0.123 | 0.68 (7.3) | .93 | 0.13 (5.4) | .98 |
| H4 | 1 | 1 | 1 | 0 | 0.095 | 0.47 (7.7) | .95 | 1.11 (5.7) | .85 |
| H5 | 0 | 0 | 0 | 1 | 0.070 | −6.9 (9.6) | .47 | −4.7 (7.1) | .50 |
| Haplotype . | VWF SNP . | . | VWF level . | FVIII level . | |||||
|---|---|---|---|---|---|---|---|---|---|
| Ile1380Val . | Asn1435Ser . | Asp1472His . | Arg2185Gln . | Freq . | β (SE) . | P value . | β (SE) . | P value . | |
| H1 | 0 | 0 | 0 | 0 | 0.500 | Referent | — | Referent | — |
| H2 | 0 | 0 | 1 | 0 | 0.210 | 13.7 (5.7) | .017 | 11.3 (4.4) | .010 |
| H3 | 0 | 0 | 1 | 1 | 0.123 | 0.68 (7.3) | .93 | 0.13 (5.4) | .98 |
| H4 | 1 | 1 | 1 | 0 | 0.095 | 0.47 (7.7) | .95 | 1.11 (5.7) | .85 |
| H5 | 0 | 0 | 0 | 1 | 0.070 | −6.9 (9.6) | .47 | −4.7 (7.1) | .50 |
β and standard error (SE) refer to the mean difference in VWF or FVIII levels for individuals carrying a single copy of the indicated haplotype compared with individuals carrying 2 copies of the referent haplotype (H1).
Freq, haplotype frequency; SE, standard error.
Discussion
Recent DNA sequencing studies of multiethnic populations found that many VWF missense variants, including some previously identified in European ancestry VWD probands (such as the type 1 and 2N variants p.Arg2185Gln and p.His817Qln), occur commonly among healthy AAs.17,18 By assessing these and other common and rare VWF coding variants in a large multicohort sample of AAs with VWF-related phenotype data, we show that 9 of 30 nonsynonymous VWF gene variants were associated with VWF:Ag, FVIII:C, or both. In multivariable-adjusted analyses, at least 6 of these variants had independent phenotypic effects on VWF:Ag and/or FVIII:C levels. As illustrated in Figure 1, the VWF-related phenotype associated missense variants tend to be localized to functional domains of VWF, such as the D′, D3, and D4 (FVIII-binding; multimerization) or A1 (platelet-binding). Notably, all VWF missense variants associated with VWF:Ag and/or FVIII:C levels in this study occur more frequently among AAs than EAs.19 Thus, our data extend recent findings on the importance of ethnic diversity of VWF sequence variants and demonstrate several of these variants may contribute to phenotypic differences in VWF:Ag and FVIII:C levels among AA.
The G allele of the common VWF rs1063856 polymorphism, which encodes the Ala form of the exon 18 p.Thr789Ala missense variant, was associated with higher VWF:Ag and FVIII:C levels in our AA sample. This finding confirms prior reports in healthy subjects and patients with diabetes of European ancestry10,11,30-33 and extends the p.Thr789Ala association to African-descent populations. rs1063856 (originally identified as an Rsa I restriction fragment length polymorphism) is in strong LD with rs1063857, which encodes a synonymous variant at p.Tyr795.34,35 In ESP AAs, the rs1063857C and rs1063856G alleles are perfectly correlated (LD r2 = 1.0). The rs1063857C/rs1063856G alleles (corresponding to p.Ala789) represent the VWF ancestral haplotype. These 2 exon 18 sites are polymorphic in all human populations studied to date; the frequency of the p.Ala789 variant varies widely from ∼70% in African to ∼40% in European to ∼5% in East Asian populations.34,36 Therefore, the worldwide pattern of allele frequency differences recapitulates the known racial/ethnic variation in VWF and FVIII levels,12-15 suggesting the p.Thr789Ala variant may account in part for the higher levels of VWF:Ag and/or FVIII:C observed in AAs.
The VWF exon 18 p.Thr789Ala polymorphism is located within the FVIII-binding D′ domain. Mutations flanking the VWF 789 residue have been implicated in type 2N VWD,7 indicating that this region serves a critical function in the VWF-FVIII interaction. Moreover, homozygosity or compound heterozygosity for a rare substitution of Pro for Ala/Thr at amino acid 789 has been reported in patients with type 2N VWD, an autosomal-recessive VWD subtype characterized by low FVIII levels due to decreased VWF-FVIII binding affinity.37 Nonetheless, the impact of p.Thr789Ala on the VWF protein is predicted to be benign and the variant does not seem to preferentially alter FVIII:C relative to VWF:Ag levels. Since p.Thr789Ala and p.Tyr795Tyr have been linked with multiple other VWF gene variants, it is plausible that other, possibly noncoding functional variants in the region encoding the D2, D′, and D3 domains are in LD or define a shared haplotype with p.Thr789Ala/p.Tyr795Tyr33 ; thus, other variants may mediate the effects attributed to p.Thr789Ala.
In our AA sample, another common African D′ domain VWF variant of exon 18, p.His817Gln (MAF = 0.11), was strongly associated with lower FVIII:C levels, disproportionately to its effect on VWF:Ag levels. p.His817Gln has been reported in 2 European patients with type 2N VWD who were compound heterozygotes for p.His817Gln and p.Arg782Trp7,38 and in 1 patient homozygous for p.His817Gln.7 In the report of Bellissimo et al,17 the mean FVIII:C level in 10 AA carriers (including 1 homozygote) was normal. Our larger sample included up to 809 heterozygotes and 52 homozygotes for the minor p.His817 allele. Therefore, the most likely reason for the discrepant results is our larger sample size and greater statistical power to detect an association for sequence variants with modest phenotypic effects. p.His817Gln is a plausible type 2N variant as it lies within the FVIII binding region and is adjacent to another type 2N variant, p.Arg816Trp.7 An in vitro study of p.His817Gln demonstrated that this amino acid change resulted in a significant decrease in FVIII binding capacity, further supporting the functional role of p.His817Gln in VWF-FVIII interaction.38
Our data confirm that the D4 domain variant p.Arg2185Gln is common in healthy AAs.17 p.Arg2185Gln was associated with lower VWF:Ag and FVIII:C levels in our large, population-based AA sample; overall, the mean VWF:Ag level in AA carriers of p.Arg2185Gln variant was 124 IU/dL compared with a mean level of 136 IU/dL in noncarriers. p.Arg2185Gln was identified in 1 subject in a series of Canadian type 1 VWD patients.39 Together, these data suggest that p.Arg2185Gln is a common functional variant associated with lower VWF:Ag and FVIII:C levels in AAs.
The missense variant p.Arg2287Trp located within the D4 domain had an allele frequency of <1% in our AA sample. This amino acid substitution was associated with a large magnitude of effect on lowering VWF:Ag levels and is predicted to be functionally deleterious (supplemental Table 2). The p.Arg2287Trp variant was reported in combination with a p.Pro2063Ser polymorphism in a European ancestry type 1 VWD patient with reduced VWF and normal FVIII and normal VWF clearance.40 Based on in vitro analysis and expression of recombinant p.Arg2287Trp missense variant, it was suggested to be a causative mutation due to a mild reduction in the amount of secreted VWF.41
Type 2M VWD is characterized by a decreased VWF activity to antigen ratio and defective binding of VWF to platelets due to mutations in the VWF A1 domain. A lower VWF activity to antigen ratio and increased prevalence of the type 2M phenotype has been reported in AAs.15,16 In AAs, the minor alleles of 3 common exon 28 A1 domain polymorphisms (p.Ile1380Val, p.Asn1435Ser, and p.Asp1472His) are present together on 1 common haplotype (frequency = 0.095), while another common allele contains p.Asp1472His with or without p.Arg2185Gln (frequency = 0.333). Flood et al16 demonstrated that p.Asp1472His alone may have the strongest association with lower VWF activity to antigen ratio. In our multivariable-adjusted regression analysis, the p.Asp1472His variant was independently associated with higher VWF:Ag levels. The haplotype containing p.Asp1472His alone was associated with higher VWF:Ag, while the Va1380/Ser1435/His1472 haplotype was not significantly associated with VWF:Ag. p.Asp1472His is located within the p.Asp1459-p.His1472 ristocetin binding site and was shown to decrease VWF ristocetin cofactor levels by affecting direct binding to ristocetin.42 Collectively, these results suggest that p.Asp1472His may lower the VWF activity to antigen ratio by lowering VWF ristocetin activity and increasing VWF:Ag levels.
p.Ser1486Leu is a novel rare variant in at a critical residue in a highly conserved cluster of 8 predicted O-glycosylation sites flanking the A1 domain43,44 that appear to modulate platelet glycoprotein Ib binding under shear stress.45 A p.Val1485Leu substitution at the adjacent amino acid (in combination with other exon 28 variants) was reported to be common among Turkish patients with VWD.46 Notably, site-directed mutagenesis of Ser1486 to Ala resulted in normal VWF synthesis and multimerization but decreased VWF hemostatic function.47 On the other hand, the substitution of Ser with Leu at 1486 is predicted to be “benign” at the protein sequence conservation level, while the substitution of Ser1486 with Ala is predicted to be “possibly damaging” by Polyphen2. Therefore, the putative mechanism of effect of the Ser1486Leu variant on lowering VWF:Ag remains to be determined.
Our data provide strong evidence that at least 6 distinct nonsynonymous VWF variants independently contribute to VWF and FVIII phenotypic differences among healthy AA individuals. In aggregate the VWF missense variants identified in our study explained 3.3% of the overall VWF phenotypic variance and 2.7% of the overall FVIII phenotypic variance. These changes are somewhat larger than the proportion of VWF phenotypic variance explained by common VWF variants in whites from the ARIC study (0.9%-1.5%).33 By comparison, ABO blood group (defined as O type vs non-O type) contributes to ∼15% of VWF:Ag phenotypic variation.33 In addition to ABO and VWF, several other genomic loci contribute to VWF:Ag and FVIII:C levels.10 Still, the total variance explained by all common variants (12.8% for VWF:Ag and 10% for FVIII:C)10 is notably less than the heritability estimates of 32% to 75% and 40% to 61% previously reported for VWF and FVIII, respectively.48 A recent linkage analysis using sibling data identified a new locus on chromosome 2 explaining 19% of additional plasma VWF variance.48 Therefore, family-based study designs and studies that include larger samples of minority participants and analysis of rare variants may help to identify “missing heritability.” The ethnic diversity of VWF coding sequence variants underscores the importance of studying ethnically diverse populations to expand our knowledge of normal genetic variation and to distinguish pathogenic changes from benign variants.17,18 Our results demonstrate that, when applied to well-characterized population-based samples, these approaches can greatly contribute to our understanding of the role of both common and rare variants to the molecular genetics of VWF-related phenotypes.
Several limitations of the current study should be noted. First, heterogeneity between laboratory assays and/or sample processing between cohorts may have introduced between-group variability. Even though the absolute values for VWF:Ag and FVIII:C differ between studies, the rank order of the values should be consistent across studies and therefore not affect the associations of high or low values with specific genetic variants. Nonetheless, interassay variability, along with variation in genotype imputation quality, may have decreased our statistical power to find associations of smaller magnitudes. Second, though none of the participants carrying common or rare VWF variants reported bleeding symptoms, a detailed clinical bleeding history was not ascertained in our cohort studies. Third, the predicted functional consequences derived from in silico sequence-conservation–based algorithms should be interpreted cautiously, since the performance of these tools can vary markedly and optimum predictions are achieved by different tools in different genes.49 Finally, it is important to point out that the bleeding tendency of VWD is a complex, incompletely penetrant phenotype. VWD is estimated to be present in up to 1% of the population, yet there is considerable overlap between individuals with low-normal VWF levels and patients diagnosed with mild type 1 VWD.50 Environmental factors and extra-allelic genetic factors that influence VWF levels, such as ABO blood group, ethnicity/genetic background, age, body mass index, pregnancy, and medications, additionally contribute to the phenotypic complexity. Application of next-generation sequence analysis in a genome-wide manner among individuals with low VWF and bleeding symptoms may help to identify cosegregating genetic variants that contribute to bleeding risk.
The online version of this article contains a data supplement.
There is an Inside Blood commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors wish to acknowledge the support of the National Heart, Lung, and Blood Institute and the contributions of the research institutions, study investigators, field staff, and study participants in creating this resource for biomedical research.
Funding for GO ESP was provided by National Institutes of Health National Heart, Lung, and Blood Institute grants RC2HL-103010 (HeartGO), RC2HL-102923 (LungGO), and RC2HL-102924 (Women's Health Initiative Sequencing Project). The exome sequencing was performed through NHLBI grants RC2HL-102925 (BroadGO) and RC2HL-102926 (SeattleGO). The WHI program is funded by the National Institutes of Health National Heart, Lung, and Blood Institute, US Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C. The NHLBI Candidate Gene Association Resource (CARE) was supported by a contract from the National Institutes of Health National Heart, Lung, and Blood Institute (HHSN268200960009C) to create a phenotype and genotype database for dissemination to the biomedical research community. Eight parent studies contributed phenotypic data and DNA samples through the Broad Institute (N01-HC-65226): the ARIC study, the Cleveland Family Study, the CARDIA study, the Jackson Heart Study, the MESA study, the Cardiovascular Health Study, the Framingham Heart Study, and the Sleep Heart Health Study. Support for CARe also came from the individual research institutions, investigators, field staff, and study participants. Individual funding information is available at http://public.nhlbi.nih.gov/GeneticsGenomics/home/care.aspx. This work was also supported in part by grants from the National Institutes of Health National Heart, Lung, and Blood Institute (R01HL71862) (A.P.R.).
Authorship
Contribution: J.M.J., P.L.A., S.S.R., and A.P.R. contributed to writing the manuscript; J.M.J., P.L.A., S.J., A.C.M., E.B., C.K., D.A.N., S.S.R., D.G., U.P., M.C., and A.P.R. provided the study concept and design; A.C.M., C.S.C., E.B., C.K., D.A.N., S.S.R., D.G., U.P., M.C., and A.P.R. acquired data; J.M.J., P.L.A., A.C.M., J.H., J.D.S., S.R.M., S.J., P.W., C.K., U.P., M.C., and A.P.R. analyzed and interpreted the data; A.C.M., S.J., P.W., K.F., N.S., C.K., S.S.R., D.G., U.P., and M.C. critically revised the manuscript for important intellectual content; C.S.C., E.B., D.A.N., S.S.R., and U.P. obtained funding; and A.P.R. supervised the study, had full access to the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Alexander P. Reiner, 1100 N Fairview Ave N M3-A410, Seattle, WA 98109; e-mail: apreiner@u.washington.edu.