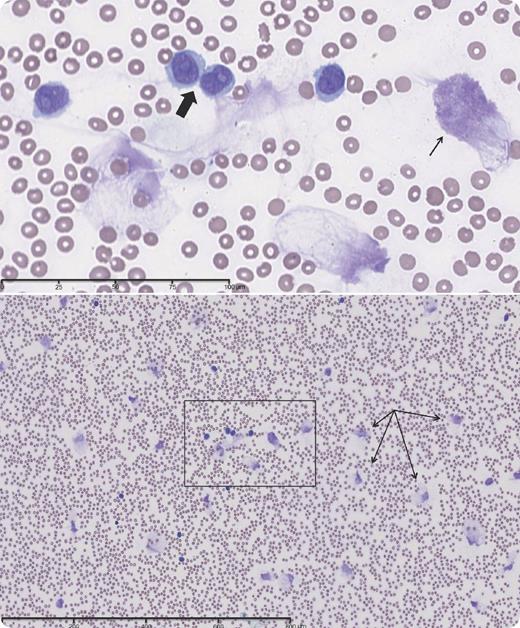
An 80-year-old white male diagnosed with de novo B-cell prolymphocytic leukemia (B-PLL) presented with increasing fatigue and moderate splenomegaly without palpable lymphadenopathy following treatment with chlorambucil. A chest CT scan showed pulmonary infiltrates, presumed to be leukemic, with a nondiagnostic bronchoalveolar lavage. The white blood cell (WBC) count was 72 × 109/L, with 82% prolymphocytes. Immunophenotyping showed that 86% of leukocytes expressed CD19, CD20, CD22, and high-density κ immunoglobulin light chain. A bone marrow biopsy showed marked infiltration by lymphocytes of variable sizes, with prominent nucleoli and lacking expression of CD5 or CD10. The peripheral blood smear showed atypical, large lymphocytes with condensed chromatin, prominent nucleoli, and abundant cytoplasm with smooth contours (bold arrow). The patient was treated with weekly pentostatin, which reduced the WBC count to 19 × 109/L. A repeat blood smear revealed numerous smudge cells (thin arrows) admixed with typical prolymphocytes.
B-PLL is a rare B-cell malignancy with a poor prognosis, distinguished from chronic lymphocytic leukemia (CLL), hairy cell leukemia, and secondary PLL arising from CLL. A diagnosis of de novo PLL requires an initial percentage of prolymphocytes >55%. This case demonstrated the tendency of circulating prolymphocytic leukemia cells to rupture during the preparation of the blood smear.
An 80-year-old white male diagnosed with de novo B-cell prolymphocytic leukemia (B-PLL) presented with increasing fatigue and moderate splenomegaly without palpable lymphadenopathy following treatment with chlorambucil. A chest CT scan showed pulmonary infiltrates, presumed to be leukemic, with a nondiagnostic bronchoalveolar lavage. The white blood cell (WBC) count was 72 × 109/L, with 82% prolymphocytes. Immunophenotyping showed that 86% of leukocytes expressed CD19, CD20, CD22, and high-density κ immunoglobulin light chain. A bone marrow biopsy showed marked infiltration by lymphocytes of variable sizes, with prominent nucleoli and lacking expression of CD5 or CD10. The peripheral blood smear showed atypical, large lymphocytes with condensed chromatin, prominent nucleoli, and abundant cytoplasm with smooth contours (bold arrow). The patient was treated with weekly pentostatin, which reduced the WBC count to 19 × 109/L. A repeat blood smear revealed numerous smudge cells (thin arrows) admixed with typical prolymphocytes.
B-PLL is a rare B-cell malignancy with a poor prognosis, distinguished from chronic lymphocytic leukemia (CLL), hairy cell leukemia, and secondary PLL arising from CLL. A diagnosis of de novo PLL requires an initial percentage of prolymphocytes >55%. This case demonstrated the tendency of circulating prolymphocytic leukemia cells to rupture during the preparation of the blood smear.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal