In this issue of Blood, authors of 2 articles have compared busulfan with total body irradiation (TBI) in preparative regimens for hematopoietic transplantation as treatment of acute myeloid leukemia (AML).1,2
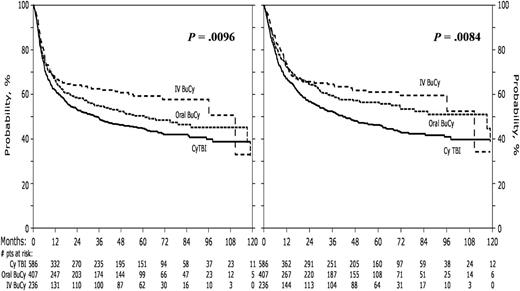
Leukemia-free survival and overall survival by preparative regimen. See Figure 2 in the article by Copelan et al that begins on page 3863.
Leukemia-free survival and overall survival by preparative regimen. See Figure 2 in the article by Copelan et al that begins on page 3863.
Myeloablative preparative regimens are designed to eradicate the leukemia and provide sufficient immunosuppression to prevent graft rejection. The optimal regimen for patients with AML is controversial. Cyclophosphamide (Cy) combined with either TBI3 or busulfan (Bu)4,5 have been widely used. A randomized study published in 1992 showed superior results with the Cy-TBI compared with Bu-Cy using the oral busulfan formulation available at that time.6 Oral busulfan is erratically absorbed, resulting in broad variation in blood levels. Busulfan systemic exposure is related to toxicities, disease control, and treatment-related mortality.7-9 An intravenous busulfan formulation has subsequently been developed, which provides more consistent pharmacokinetics and reliable dosing10 ; it may also avoid first-pass hepatotoxicity related to oral dosing. Intravenous busulfan has largely replaced the oral formulation in preparative regimens for hematopoietic transplantation.
These 2 articles directly compare busulfan and TBI for hematopoietic transplantation as treatment of AML in the modern era. Copelan et al performed a retrospective review of 1230 patients with AML in first complete remission reported to the Center for International Blood and Marrow Transplantation Research receiving Cy-TBI or Bu-Cy with either the oral or intravenous busulfan formulation between 2000 and 2006.1 By multivariate analysis, they report significantly less nonrelapse mortality and relapse after 1 year posttransplant and better leukemia-free and overall survival for those receiving intravenous, but not oral, Bu-Cy compared with Cy-TBI. Similar conclusions applied to TBI given with standard fractionation or in higher doses. Thus, these data indicate reduced toxicity and improved survival with the intravenous Bu-Cy regimen compared with Cy-TBI. Leukemia-free survival and survival is shown in the figure.
Bredeson et al performed a second “prospective” nonrandomized cohort study between 2009 and 2011, testing the noninferiority of survival with intravenous busulfan vs TBI-based myeloablative preparative regimens for hematopoietic transplantation for myeloid malignancies.2 A total of 1483 patients were enrolled; most had AML. Cohorts were balanced for prognostic factors impacting outcome. For AML patients, 2-year survival was 57% with busulfan and 46% with TBI-based regimens; P = .003. The only concern of note was a higher incidence of hepatic venoocclusive disease for Bu (5%) than with TBI (1%). There were no differences in progression-free survival and graft-versus-host disease. The combination of busulfan and fludarabine has been studied as a potentially less toxic alternative to busulfan-cyclophosphamide.11,12 The Bredeson study also compared patients receiving busulfan-fludarabine vs busulfan-cyclophosphamide; there was no difference in outcomes with these preparative regimens.
Together, these 2 studies indicate improved survival in patients receiving a preparative regimen using intravenous busulfan compared with TBI for myeloablative hematopoietic transplantation as treatment of AML. Ideally, this should be confirmed by a randomized controlled trial, but a similarly sized randomized trial is not feasible. The available data indicate that, compared with myeloablative TBI, a preparative regimen using intravenous busulfan is relatively safe and effective for treatment of AML, and thus it should be considered a standard of care for allogeneic hematopoietic transplantation in these patients.
Conflict-of-interest disclosure: R.E.C. received a research grant from Otsuka Corporation.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal