In this issue of Blood, Yao and colleagues describe mice with vascular endothelial cell (EC) deletion of gp130, a signaling subunit for the interleukin-6 (IL-6) family of cytokines.1 The authors postulated that such mice would exhibit an attenuated response to inflammatory stimuli but, surprisingly, the opposite phenotype was observed. These mice exhibited a dysregulated CXCL1 chemokine gradient in the endothelium, leading to neutrophils that stuck to the apical endothelial surface and were unable to exit the vessel lumen.
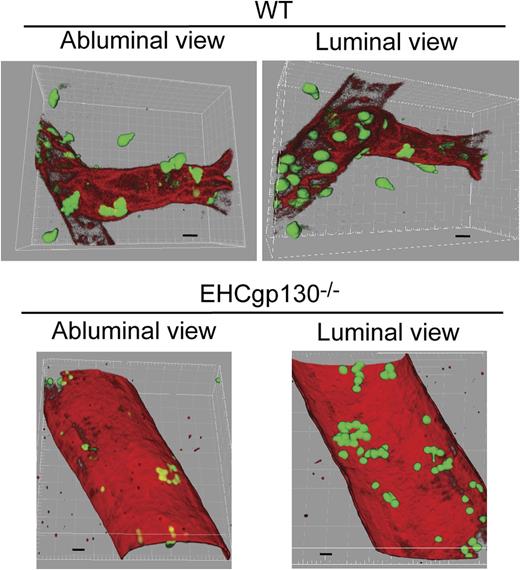
Three-dimensional reconstructions of confocal microscopy images of TNF-α–activated venules of cremaster microcirculation from WT (top) and EHCgp130–/– mice (bottom). Adherent neutrophils are shown in green. Note that in venules of WT mice, the luminal side has many adherent neutrophils and the basolateral side contains several neutrophils that have exited the vessel. Most neutrophils have migrated into the interstitial space well beyond the vessel. In contrast, the venules of the EHCgp130−/− mice contains neutrophils adherent to the luminal surface but very few neutrophils that have exited the vessel. See Figure 5E in the article by Yao et al, which begins on page 3832.
Three-dimensional reconstructions of confocal microscopy images of TNF-α–activated venules of cremaster microcirculation from WT (top) and EHCgp130–/– mice (bottom). Adherent neutrophils are shown in green. Note that in venules of WT mice, the luminal side has many adherent neutrophils and the basolateral side contains several neutrophils that have exited the vessel. Most neutrophils have migrated into the interstitial space well beyond the vessel. In contrast, the venules of the EHCgp130−/− mice contains neutrophils adherent to the luminal surface but very few neutrophils that have exited the vessel. See Figure 5E in the article by Yao et al, which begins on page 3832.
It is now well documented that at sites of inflammation, the vascular endothelium becomes “activated” by proinflammatory cytokines (eg, IL-6Rα/IL-6, oncostatin M, IL-1β, tumor necrosis factor [TNF]-α), bacterial endotoxins, and other inflammatory stimuli. Upon activation, the endothelium rapidly converts from a nonadhesive vascular lining to become proadhesive by transcriptional upregulation of surface adhesion molecules and production of chemokines that capture and recruit blood leukocytes.2 The activated endothelium confers spatial and temporal localization and leukocyte-type selectivity to the inflammatory response. Successful leukocyte transmigration across postcapillary venules in tissues is the culmination of multiple adhesive steps mediated by multiple classes of adhesion molecules expressed on the surface of the ECs and their interaction with blood leukocytes.3 Studies performed in the early 1990s using intravital microscopy of rabbit mesenteric venules were the first to describe a multistep model of neutrophil recruitment: leukocyte rolling via l-selectin (step 1) and firm adhesion via β2 integrins (step 2).4 EC-expressed chemoattractants or chemokines mediate the arrest step and are thought to promote subsequent leukocyte transmigration between (paracellular) or through (transcellular) the vascular endothelium. Once beneath the endothelium, other cells including pericytes, interstitial neutrophils, activated macrophages, and fibroblasts have been shown to produce a relay system of chemoattractants or chemokines that form gradients to promote neutrophil-directed migration away from the vessel and toward another gradient of attractants that originate from the site of inflammation or injury. However, what happens when the vascular endothelium vastly overexpresses and stores a chemokine that recruits primarily neutrophils?
As reported in this issue of Blood, Yao and colleagues created mice with EC-specific deletion of gp130, a signaling subunit for the IL-6 family of proinflammatory cytokines.1 Their hypothesis was that loss of gp130 would “short circuit” EC activation in response to oncostatin M or IL-6/IL6Rα complexes, thus preventing activation of ECs and subsequent leukocyte recruitment. Surprisingly, these mice (EHCgp130−/−) expressed dramatically elevated levels of messenger RNA and protein for CXCL1 specifically in ECs but, counterintuitively, the mice have a significant defect in neutrophil recruitment in models of inflammation of the cremaster muscle microcirculation and in thioglycollate-induced peritonitis. The actual mechanism was quite unexpected, namely robust neutrophil arrest but severely reduced transendothelial migration, and was thoroughly vetted by these investigators using a variety of approaches.
Upon TNF-α–induced activation of the cremaster muscle microcirculation of wild-type (WT) mice, many neutrophils roll on the apical surface, arrest, transmigrate across the endothelium, and exit from the venule into the interstitial space. In contrast to WT mice, the endothelium in EHCgp130−/− mice was carpeted with firmly “stuck” neutrophils that were unable to transmigrate and remained stably bound (see figure), and few rolling neutrophils were observed. The arrest step was prevented by antibody inhibition of β2 integrins. The authors reported that the “stuck” neutrophils failed to exit the venules. Moreover, superfusion of CXCL1 or a potent formyl peptide chemoattractant of venules in EHCgp130−/− mice did not encourage stuck leukocytes to transmigrate across the endothelium, suggesting that neutrophil β2 integrins were locked in a high affinity conformation and unable to release from their EC ligand ICAM-1. A second model, using surgical induced trauma in the cremaster, revealed a similar difference in neutrophil adhesion between WT and EHCgp130−/− mice. WT mice vessels supported significant rolling of leukocytes, but few stably adherent cells.5 In contrast, EHCgp130−/− mice exhibited numerous stably adherent leukocytes, with few rolling leukocytes in cremaster venules. It is worthwhile to point out that the markedly increased basal production of CXCL1 by EHCgp130−/− ECs was not secreted into the blood but was instead stored in intracellular compartments. The stored CXCL1 could be mobilized by surgical trauma or TNF-α, thereby enhancing neutrophil arrest. A caveat of the EHCgp130−/− mice is that they lack gp130 in endothelial and hematopoietic cells,6 which occurs when Tie2-Cre mice are used. Studies were performed that ruled out a contribution from neutrophil gp130. Taken together, these experiments demonstrated that the gp130 deficiency in the endothelium, not in leukocytes, is responsible for excess firm adhesion of neutrophils in venules.
In summary, the take-home message from this article is that loss of EC gp130 gene alters transcriptional regulation of CXCL1. In TNF-α– or thioglycollate-induced acute inflammation, EC activation leads enhanced CXCL1 production and apical presentation and enhanced neutrophil arrest but impaired transendothelial cell migration in vivo and in vitro. This study raises a number of interesting questions regarding the phenotype of EHCgp130−/− in models of acute bacterial inflammation. Are these mice more susceptible to sublethal acute bacterial challenge? Normally during the inflammatory response, the first responders are neutrophils and the subsequent responders are typically monocytes and macrophages, followed by formation of granulation tissue and healing to regenerate the tissue or organ. Do EHCgp130−/− mice have an abnormal inflammatory response in chronic models of inflammation or after specific organ (eg, heart, lung, liver, kidney) insult? Is tissue or organ regeneration normal or altered? CXCL1 has been implicated in angiogenesis in a variety of murine models. Do the ECs from EHCgp130−/− mice have an abnormal angiogenic response? It is also interesting why the loss of gp130 in ECs leads to dysregulated transcription of the CXCL-1 gene. Finally, it would be of interest to generate mice with conditional, EC-specific deletion of the gp130 gene to address certain of these issues.
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal