Abstract

Five-year overall survival (OS) of chronic myeloid leukemia (CML) patients treated with imatinib exceeds 90%. With many tyrosine kinase inhibitors (TKI) available as treatment options for CML, the influence of TKI therapy on OS is difficult to define. Comorbidities can complicate randomized trials. Their influence on OS in CML has not been studied so far.
We sought to evaluate the influence of comorbidities at diagnosis of CML on remission rates and OS of patients with Philadelphia and/or BCR-ABL positive chronic-phase CML. The CML-Study IV, a randomized five-arm trial designed to optimize imatinib therapy alone or in combination, used very few exclusion criteria as compared to other studies which typically excluded patients with severe illnesses.
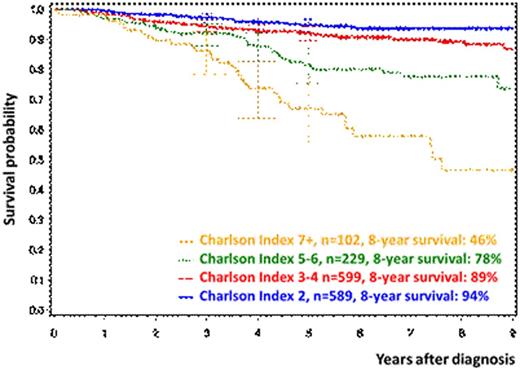
The age-adjusted Charlson Comorbidity Index (CCI) is the most extensively studied comorbidity index (Charlson ME et al., 1987) and has been validated for long-term studies. The score weighs a) the severity of comorbidities (e.g. one point is allocated to myocardial infarction and diabetes, two points to non-active malignancies) and b) the age of patients (with one point for each decade above 40 years). The CCI at diagnosis was calculated for each randomized patient. For the analyses, patients were grouped into CCI 2, 3-4, 5-6, and ≥7. Performance status was measured by the Karnofsky Score (KS) and patients were grouped into 50-80, >80-<100, and 100. Correlation analyses were performed by the chi-square test. Survival probabilities were calculated by Kaplan-Meier curves. Calculating cumulative incidences, the competing risks progression and/or death were considered. Cox models were estimated for the multivariate analysis to analyse the prognostic influence of the candidate factors age, sex, leukocytes, hemoglobin, EUTOS score, KS, and CCI on OS.
1551 patients were randomized from 2002 to 2012, 1524 patients were evaluable. Median follow-up time was 67.5 months. Additional to CML, 521 index comorbidities were reported in 1519 patients resulting in the following CCI groups: i) CCI 2: 589 patients, ii) CCI 3 or 4: 599 patients, iii) CCI 5 or 6: 229 patients, and iv) CCI ≥ 7: 102 patients. Median value of the CCI was 3 (range: 2-12). The distribution of the CCI groups was not different between treatment arms. Most common comorbidities were diabetes (n=106), non-active cancer (n=102), chronic pulmonary disease (n=74), renal insufficiency (n=47), myocardial infarction (n=38), cerebrovascular disease (n=29), congestive heart failure (n=28), and peripheral vascular disease (n=28).
Between patients with CCI 2, 3-4, 5-6, and ≥7 no significant differences in remission rates were found neither for time to complete cytogenetic remission (CCR) nor for time to major molecular remission (MMR). Median times to CCR were 12.9, 12.6, 13.7, and 13.1 months and to MMR 17.5, 15.9, 16.5, and 18.1 months, respectively. No differences were observed between the CCI groups for the cumulative incidences of progression. As expected, significant differences in OS according to CCI at diagnosis were observed (s. Fig. 1, p<0.001). Probabilities of OS at 8 years for patients with CCI 2, 3-4, 5-6, and ≥7 were 93.6%, 89.4%, 78.7%, and 45.2%.
We found a correlation between CCI and KS (p<0.001). In multivariate analysis CCI (p<0.001), KS (p=0.022), and EUTOS Score (p=0.012) were significant predictors of OS. Hazard ratios for the CCI group 3-4, 5-6, >7 (each vs. 2), were 1.695 (95%-confidence interval, CI 1.066-2.695), 3.231 (CI 1.942-5.376) and 6.495 (CI 3.817-11.111), respectively. Separating the CCI into an age-related part and a comorbidity-related part, the comorbidity-related part was still an important risk factor (Wald test, p=0.002).
Comorbidities of CML-patients do not seem to have an impact on the success of imatinib treatment. In CML-Study IV, even patients with a considerable comorbidity benefitted from imatinib as the chances to achieve MMR and CCR did not differ from those of healthier CML-patients. Our data also indicate that OS alone is not any more an appropriate measure for the effectiveness of a specific treatment for CML, as TKI have reduced the CML-related lethality to too low levels. Adjusting for comorbidity is essential for a valid comparison and interpretation of OS observed with different TKIs in CML-patients.
Saussele:Pfizer: Honoraria; BMS: Honoraria, Research Funding, Travel, Travel Other; Novartis: Honoraria, Research Funding, Travel Other. Hehlmann:BMS: Consultancy, Research Funding; Novartis: Research Funding. Hochhaus:Novartis: Consultancy, Honoraria, Research Funding, Travel Other; BMS: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria; Ariad: Consultancy, Honoraria. Müller:Ariad: Honoraria; BMS: Honoraria, Research Funding; Novartis: Honoraria, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal