Abstract
Cytotoxic T Lymphocyte Antigen 4 (CTLA4) is a critical T cell molecule that inhibits T cell activation and plays an essential role in T cell homeostasis and immune responses. Genetic variations in the CTLA4 gene have been hypothesized to be possible biologic markers that are predictive of transplant outcomes. Previous investigators have studied single nucleotide polymorphisms (SNPs) of the CTLA4 gene and its impact on hematopoietic cell transplantation (HCT) outcomes with discordant results. AA and AG genotypes in the donor CTLA4 regulatory region involving SNP rs4553808 in patients after unrelated donor (URD) HCT have recently been shown to be an independent predictor of improved relapse free survival (RFS) and overall survival (OS) compared to the GG genotype. To validate these preliminary findings, a Center for International Blood and Marrow Research (CIBMTR) study was performed in a larger, more homogenous cohort of patients.
Adult patients with acute myeloid leukemia (AML) and advanced myelodysplastic syndrome (MDS) undergoing a first 8/8 or 7/8 HLA matched URD HCT after myeloablative, non-myeloablative, or reduced intensity conditioning from 2002 to 2007 in first or second complete remission with available donor research samples from the National Marrow Donor Program research repository were included. The primary goal was to evaluate the impact of SNP rs4553808 on RFS, OS, and NRM and the cumulative incidence of acute graft-versus-host disease (aGVHD), and chronic graft-versus-host disease (cGVHD). Any GVHD prophylaxis could be used except in vitro T-cell depletion or use of in vivo/in vitro alemtuzumab. Patients receiving T cell depletion with anti-thymocyte globulin (ATG) were oversampled to allow analysis of any effects on outcomes. An exploratory analysis of 9 other tagSNPs that encompass the entire CTLA4 gene (rs231775, rs231779, rs11571315, rs231777, rs3087243, rs16840252, rs231725, rs10197010, rs11571316) was performed to evaluate for any additional potential associations with clinical outcomes.
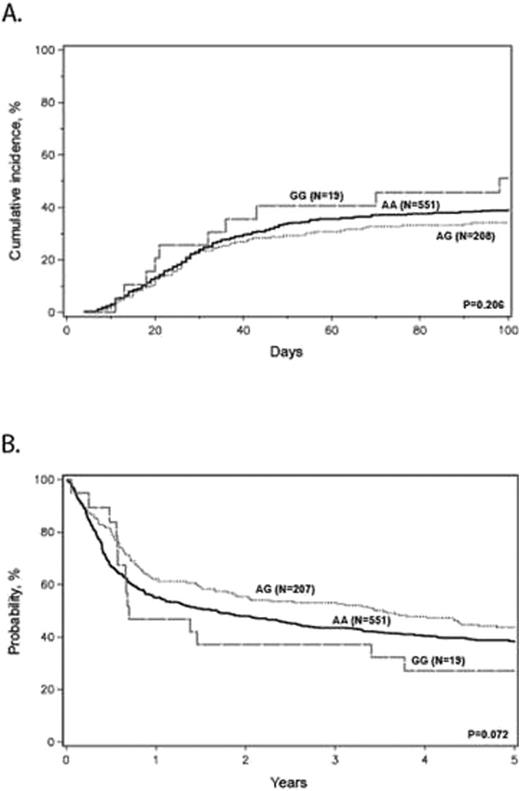
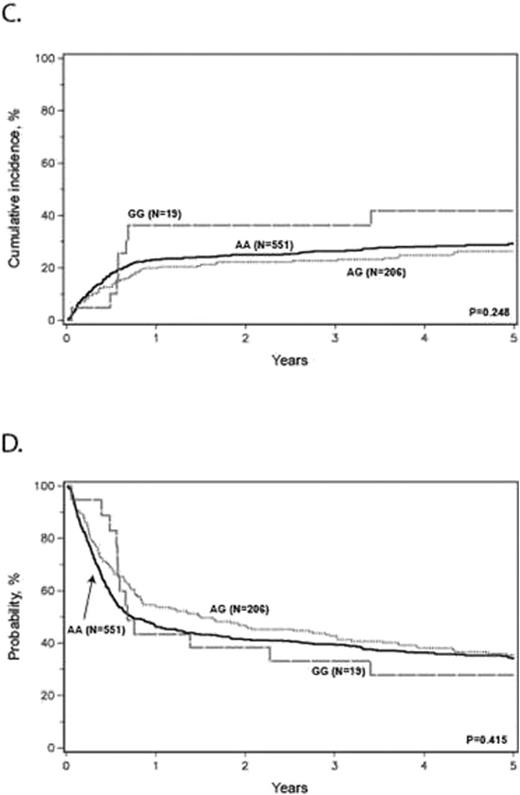
(A) adjusted cumulative incidence of grades 2-4 aGVHD, (B) adjusted probability of overall survival, (C) adjusted cumulative incidence of non-relapse mortality, (D) adjusted probability of relapse free survival stratified by donor CTLA4 SNP rs4553808 genotype.
(A) adjusted cumulative incidence of grades 2-4 aGVHD, (B) adjusted probability of overall survival, (C) adjusted cumulative incidence of non-relapse mortality, (D) adjusted probability of relapse free survival stratified by donor CTLA4 SNP rs4553808 genotype.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal