Abstract
Perceived discrimination due to race or ethnicity has been associated with a greater burden of pain among minority groups. Patients with sickle cell disease (SCD), who in the U.S. are comprised primarily of individuals from racial and ethnic minority groups, are known to experience behaviors from others that may be construed as discriminatory. Nevertheless, the association of these problematic interpersonal experiences with the burden of chronic pain in SCD is unknown.
We conducted a cross-sectional analysis of data collected at baseline of the Improving Patient Outcomes with Respect and Trust Study (IMPORT), which is a federally funded prospective cohort study of SCD patient (age 15+) experiences of care (n = 291). We sought to examine the association between patient perceptions of discrimination and their reports of chronic SCD pain. Perceived discrimination from healthcare providers thought to be due to the patient's race/ethnicity (i.e., race-based), or status as having SCD (i.e, disease-based) was measured using subscales adapted from the Interpersonal Processes of Care Survey. Using descriptive, bivariate, and multivariable analytic techniques, discrimination scores were examined for their association with self-reported chronic pain both unadjusted, and adjusted for the following potential confounders: patient age, sex, type of SCD, self-reported ED utilization for vaso-occlusive crisis, depression symptoms, the patient's perceived severity of their SCD, and the presence or absence of avascular necrosis.
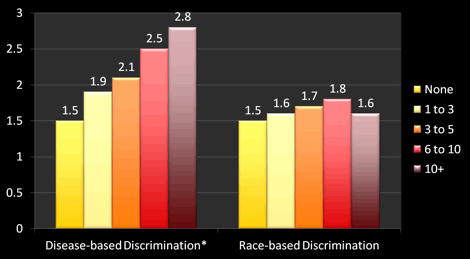
Patients in the cohort reported higher levels of race-based discrimination compared to other reports of African Americans using the same instrument. The cohort reported an even higher level of perceived disease-based discrimination than race-based discrimination. Race-based discrimination exhibited significant, positive associations with disease-based discrimination (r = 0.51, p<0.001), age, and depressive symptoms. Disease-based discrimination exhibited significant, positive associations with depressive symptoms, ED utilization (see Figure 1), and perceived disease severity. Fifty-four percent (54%) of the respondents reported having daily chronic SCD pain. Perceived disease-based, but not race-based, discrimination from healthcare providers was independently associated with a greater likelihood of reporting daily chronic SCD pain (adjusted OR = 1.34, 95%CI [1.01, 1.78]) after adjustment for all potential confounders under study.
While perceptions of race and disease-based discrimination were correlated with each other, they exhibited different relationships with clinical factors like ED utilization and chronic pain. Perceived disease-based, but not race-based, discrimination was found to be associated with a greater burden of chronic pain among patients with SCD independent of potential confounders like ED utilization. While the true causal directionality of this relationship is currently unclear, our findings do support greater use of a biopsychosocial approach to mitigating the burden of SCD pain. Efforts to identify the various mechanisms through which perceived discrimination is associated with the burden of pain are essential in order to develop targeted interventions that could improve the pain experience of persons with SCD.
* Test for trend significant at p <0.001
Haywood:NIH: Research Funding. Lanzkron:GlycoMimetics, Inc: Research Funding; NIH: Research Funding. Strouse:NIH: Research Funding; Doris Duke Charitable Foundation: Research Funding; Masimo Corporation: Membership on an entity’s Board of Directors or advisory committees, Research Funding. Bediako:NIH: Research Funding. Haythornthwaite:NIH: Research Funding. Beach:NIH: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal